Key Takeaways
- Rhabdomyosarcoma is a rare cancer of soft tissue, primarily affecting children and adolescents, originating from immature muscle cells.
- Symptoms vary widely depending on the tumor’s location, often presenting as a painless mass or swelling.
- Diagnosis typically involves imaging, biopsy, and pathological examination to determine the specific types of rhabdomyosarcoma cancer.
- Treatment is multimodal, combining surgery, chemotherapy, and radiation therapy, tailored to the individual patient and tumor characteristics.
- Significant advancements in treatment and latest research rhabdomyosarcoma have improved outcomes, particularly for rhabdomyosarcoma in children.
What is Rhabdomyosarcoma?
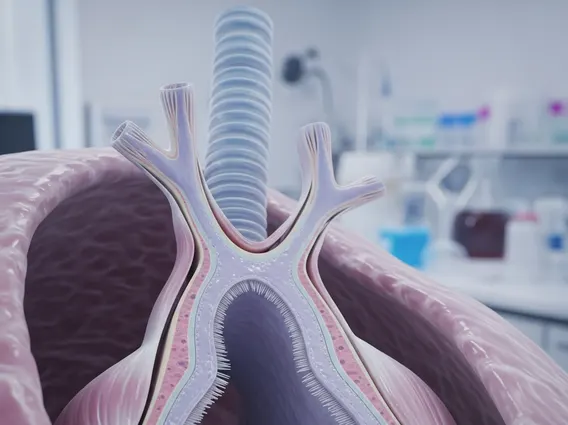
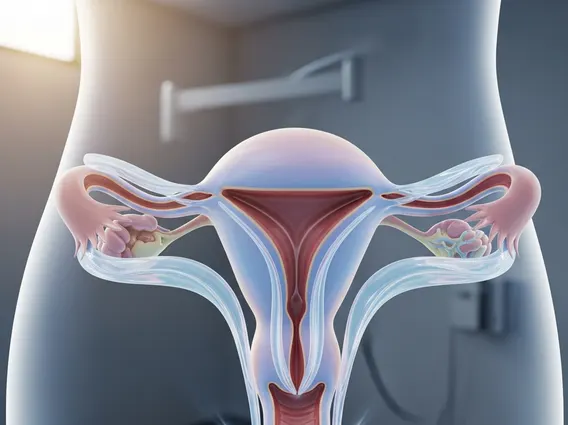
Rhabdomyosarcoma is a malignant tumor that arises from mesenchymal cells, which are primitive cells that normally develop into skeletal muscle. This cancer can develop in various parts of the body where skeletal muscle or its precursor cells are found, including the head and neck, genitourinary tract, extremities, and trunk. It is the most common soft tissue sarcoma in children, accounting for approximately 3% of all childhood cancers. According to the American Cancer Society, about 350 new cases of RMS are diagnosed in the United States each year, with the majority occurring in those under 18 years old.
Key Characteristics and Types
The defining characteristic of rhabdomyosarcoma is its origin from rhabdomyoblasts, which are embryonic cells that would normally differentiate into striated muscle. The aggressiveness and treatment approach for RMS often depend on its specific subtype and location.
There are several types of rhabdomyosarcoma cancer, each with distinct cellular features and clinical behaviors:
- Embryonal Rhabdomyosarcoma (ERMS): This is the most common type, accounting for about 60-70% of all RMS cases. It typically affects infants and young children and often occurs in the head and neck region (especially around the eye), genitourinary tract, or retroperitoneum. A variant of ERMS, known as botryoid rhabdomyosarcoma, grows in a grape-like cluster and is often found in hollow organs like the bladder or vagina.
- Alveolar Rhabdomyosarcoma (ARMS): Representing about 20-25% of cases, ARMS is more common in older children and adolescents. It frequently arises in the limbs, trunk, or perineum. This subtype is generally more aggressive than ERMS and often associated with specific chromosomal translocations, such as t(2;13) or t(1;13), which are important for diagnosis and prognosis.
- Pleomorphic Rhabdomyosarcoma (PRMS): This type is rare in children and primarily affects adults. It typically occurs in the extremities and is characterized by highly pleomorphic (variably shaped) tumor cells.
- Spindle Cell/Sclerosing Rhabdomyosarcoma: A more recently recognized subtype, it can occur in both children and adults. It is characterized by spindle-shaped cells and a sclerotic (hardened) background, and its prognosis can vary.
Recognizing Symptoms and Underlying Causes
Understanding rhabdomyosarcoma symptoms and causes is crucial for early detection, although the symptoms can be non-specific and vary greatly depending on the tumor’s location and size. There are no definitive known causes for the majority of RMS cases, but certain genetic predispositions have been identified.
Common symptoms often include:
- Painless Mass or Swelling: This is the most frequent symptom, appearing as a lump that may grow rapidly. Its location dictates other symptoms. For instance, a tumor in the head and neck might cause eye bulging (proptosis), difficulty swallowing, or nasal obstruction.
- Pain: While often painless initially, as the tumor grows and presses on nerves or other structures, it can cause localized pain.
- Neurological Symptoms: Tumors near the brain or spinal cord can lead to headaches, vision changes, weakness, or numbness.
- Urinary or Bowel Issues: If the tumor is in the genitourinary tract, symptoms may include blood in the urine, difficulty urinating, or constipation.
- Systemic Symptoms: In advanced stages, or with widespread disease, patients might experience unexplained weight loss, fever, or fatigue.
Regarding underlying causes, most cases of rhabdomyosarcoma occur sporadically, meaning they are not inherited and have no clear cause. However, a small percentage of individuals with RMS may have inherited genetic syndromes that increase their risk. These include:
- Li-Fraumeni Syndrome: Caused by mutations in the TP53 tumor suppressor gene.
- Neurofibromatosis Type 1 (NF1): A genetic disorder that affects nerve tissue growth.
- Beckwith-Wiedemann Syndrome: A growth disorder associated with an increased risk of several childhood cancers.
- Noonan Syndrome: A genetic condition characterized by unusual facial features, short stature, heart defects, and other physical problems.
Environmental factors have not been definitively linked to the development of RMS, and research continues to explore potential contributing elements.
Diagnosis and Treatment Approaches
Effective management of rhabdomyosarcoma diagnosis and treatment requires a multidisciplinary approach, involving oncologists, surgeons, radiation therapists, pathologists, and other specialists. The goal is to accurately identify the cancer, determine its extent, and apply the most effective combination of therapies.
Diagnostic Methods
The diagnostic process for rhabdomyosarcoma typically begins with a thorough physical examination and medical history. Subsequent steps are crucial for confirming the diagnosis and staging the disease:
- Imaging Studies: Techniques such as MRI (Magnetic Resonance Imaging), CT (Computed Tomography) scans, PET (Positron Emission Tomography) scans, and ultrasound are used to visualize the tumor, assess its size and local extent, and check for spread to other parts of the body. Bone scans may also be performed to detect bone involvement.
- Biopsy: A definitive diagnosis of RMS requires a tissue biopsy, where a small sample of the tumor is removed and examined under a microscope by a pathologist. This is critical for identifying the specific subtype of rhabdomyosarcoma and can also involve genetic testing for characteristic chromosomal translocations (e.g., in alveolar RMS).
- Bone Marrow Aspiration and Biopsy: These procedures are performed to check for cancer cells in the bone marrow, which is important for staging.
- Lumbar Puncture: If the tumor is located near the central nervous system, a lumbar puncture (spinal tap) may be performed to check for cancer cells in the cerebrospinal fluid.
Once diagnosed, the cancer is staged, which helps guide treatment decisions. Staging considers the tumor’s size, location, whether it has spread to lymph nodes, and if it has metastasized to distant sites.
Treatment Modalities
Treatment for rhabdomyosarcoma is highly individualized and typically involves a combination of therapies:
| Treatment Modality | Description |
|---|---|
| Surgery | Aims to remove as much of the tumor as safely possible. For localized tumors, complete surgical removal (resection) is often the primary goal. In some cases, if the tumor is large or in a difficult location, surgery may be performed after chemotherapy to shrink the tumor. |
| Chemotherapy | Uses powerful drugs to kill cancer cells throughout the body. It is a cornerstone of RMS treatment, often administered before (neoadjuvant), during, and after (adjuvant) other treatments. Common chemotherapy drugs include vincristine, dactinomycin, cyclophosphamide, and doxorubicin. |
| Radiation Therapy | Uses high-energy X-rays or other types of radiation to kill cancer cells or stop them from growing. It is often used for tumors that cannot be completely removed surgically, or to target microscopic disease after surgery. Proton therapy, a type of radiation, may be used to reduce damage to surrounding healthy tissues, especially in children. |
| Targeted Therapy | Newer treatments that specifically target cancer cells based on their genetic mutations or molecular characteristics, while minimizing harm to normal cells. These are often used in clinical trials or for recurrent/refractory cases. |
The specific combination and sequence of these treatments depend on the tumor’s type, location, stage, and the patient’s age and overall health.
Rhabdomyosarcoma in Pediatric Patients
Rhabdomyosarcoma in children presents unique challenges and considerations due to the developing nature of their bodies. It is the most common soft tissue sarcoma in children and adolescents, with approximately two-thirds of all cases diagnosed before the age of 10. The incidence peaks in two age groups: infants and toddlers (ages 1-5) and adolescents (ages 10-18).
Treating RMS in pediatric patients requires careful planning to minimize long-term side effects while maximizing treatment efficacy. Children are more susceptible to the long-term toxicities of chemotherapy and radiation, which can affect growth, development, fertility, and increase the risk of secondary cancers. Therefore, treatment protocols are often adapted to reduce these risks, utilizing lower doses or more targeted approaches where possible.
Pediatric oncology centers specialize in treating childhood cancers and offer comprehensive care that addresses not only the cancer itself but also the developmental, psychological, and social needs of young patients and their families. Clinical trials play a significant role in advancing treatment for children with RMS, providing access to cutting-edge therapies and improving outcomes.
Prognosis and Advancements in Research
The rhabdomyosarcoma prognosis and survival rates have significantly improved over the past few decades, largely due to advancements in multimodal therapy and a better understanding of the disease. Prognosis is highly variable and depends on several factors, including the tumor’s subtype, location, size, stage at diagnosis, and the patient’s age.
- Localized Disease: For patients with localized embryonal rhabdomyosarcoma that can be completely removed, survival rates can be as high as 70-80%.
- Regional Spread: If the cancer has spread to nearby lymph nodes, the prognosis is less favorable but still significantly improved with aggressive treatment.
- Metastatic Disease: For patients with metastatic RMS (cancer that has spread to distant parts of the body), the prognosis remains challenging, with survival rates generally lower, though still improving with intensive therapy.
- Alveolar Subtype: Alveolar rhabdomyosarcoma generally has a less favorable prognosis compared to embryonal rhabdomyosarcoma, especially if it carries certain genetic translocations.
Long-term follow-up is essential for RMS survivors to monitor for recurrence and manage potential late effects of treatment, such as cardiac issues, secondary malignancies, or fertility problems.
The latest research rhabdomyosarcoma is focused on several promising areas aimed at further improving outcomes and reducing treatment toxicities:
- Genomic Profiling: Detailed analysis of the genetic and molecular characteristics of RMS tumors is helping to identify new therapeutic targets and develop personalized treatment strategies.
- Targeted Therapies: Researchers are investigating drugs that specifically block molecular pathways crucial for RMS growth and survival, such as inhibitors of receptor tyrosine kinases (e.g., IGF-1R inhibitors) or cell cycle regulators.
- Immunotherapy: Exploring the use of the body’s own immune system to fight cancer, including checkpoint inhibitors and CAR T-cell therapy, is a rapidly evolving field with potential applications for RMS.
- Improved Radiation Techniques: Advances in radiation delivery, such as proton therapy, aim to precisely target tumors while sparing healthy tissues, thereby reducing long-term side effects, particularly in growing children.
- Drug Delivery Systems: Developing novel methods to deliver chemotherapy drugs more effectively to tumor sites, potentially reducing systemic toxicity.
These ongoing research efforts offer hope for continued improvements in the treatment and long-term survival for individuals affected by rhabdomyosarcoma.
Rhabdomyosarcoma primarily affects children and adolescents. While it can occur at any age, the majority of cases are diagnosed in individuals under 18 years old, with peaks in incidence observed in infants and toddlers (ages 1-5) and again in adolescents (ages 10-18). It is considered the most common soft tissue sarcoma in the pediatric population.
Yes, there are several types of rhabdomyosarcoma, with Embryonal Rhabdomyosarcoma (ERMS) and Alveolar Rhabdomyosarcoma (ARMS) being the most common. ERMS generally has a more favorable prognosis and typically affects younger children, often in the head and neck or genitourinary tract. ARMS is usually more aggressive, common in older children and adolescents, and frequently found in the limbs or trunk, often associated with specific genetic translocations that can influence prognosis.
Treatment for rhabdomyosarcoma is typically multimodal, combining surgery, chemotherapy, and radiation therapy. Surgery aims to remove the tumor, while chemotherapy uses drugs to kill cancer cells throughout the body. Radiation therapy uses high-energy beams to target and destroy cancer cells locally. The specific combination and sequence of these treatments are tailored based on the tumor’s type, location, stage, and the patient’s overall health.