Pleuropulmonary Blastoma
Pleuropulmonary Blastoma (PPB) is an exceptionally rare and aggressive childhood cancer that originates in the lungs and the surrounding pleura. Understanding this complex disease is crucial for early diagnosis and effective management, given its unique characteristics and potential genetic links.
Key Takeaways
- Pleuropulmonary Blastoma is a rare and aggressive cancer primarily affecting infants and young children, originating in the lungs and pleura.
- The majority of cases are linked to germline mutations in the DICER1 gene, indicating a strong genetic predisposition.
- Symptoms are often non-specific, including cough, shortness of breath, and fever, making early diagnosis challenging.
- Treatment typically involves a multidisciplinary approach, combining surgery, chemotherapy, and sometimes radiation therapy.
- Prognosis varies significantly depending on the tumor type and stage at diagnosis, highlighting the need for specialized care.
What is Pleuropulmonary Blastoma?
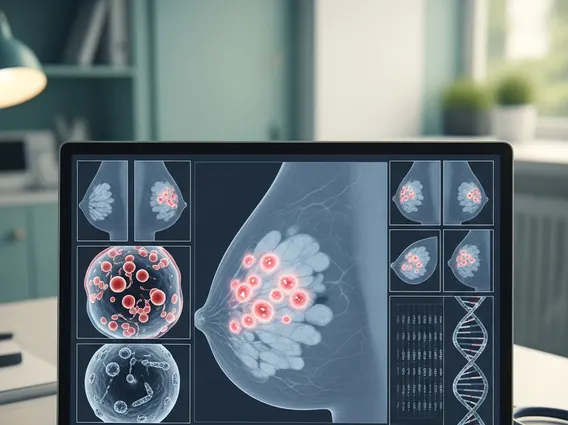
Pleuropulmonary Blastoma (PPB) is a malignant tumor that develops in the lungs and/or pleura (the lining around the lungs) of infants and young children. It is classified into different types (Type I, Ir, II, and III) based on its histological features and aggressiveness, with Type I being the least aggressive and Type III the most aggressive. This rare cancer typically manifests before the age of seven, with most diagnoses occurring in children under five years old. Its rarity means that specialized medical centers with experience in pediatric oncology are best equipped to manage its diagnosis and treatment.
The incidence of PPB is estimated to be approximately 1 in 200,000 to 300,000 live births, making it one of the rarest forms of childhood cancer. According to data from the International PPB Registry, Type I and Ir tumors are often cystic, while Type II and III tumors are solid and tend to be more aggressive, requiring intensive treatment strategies. Early and accurate classification is vital for determining the most appropriate therapeutic approach and predicting prognosis.
Causes and Symptoms of Pleuropulmonary Blastoma
The primary pleuropulmonary blastoma causes are often linked to genetic mutations. A significant proportion of children with PPB, particularly those with Type I and II tumors, have a germline mutation in the DICER1 gene. This gene plays a crucial role in microRNA processing, which is essential for normal cell development. Mutations in DICER1 can lead to a predisposition to various tumors, including PPB, ovarian Sertoli-Leydig cell tumors, and thyroid nodules, a condition known as DICER1 syndrome. Family members of affected individuals may also carry the mutation, necessitating genetic counseling and screening. The DICER1 gene mutation is found in about 70-80% of PPB cases, as reported by the National Cancer Institute.
The pleuropulmonary blastoma symptoms can be non-specific and often mimic more common childhood respiratory illnesses, making early diagnosis challenging. Symptoms typically depend on the tumor’s size, location, and whether it’s compressing surrounding structures. Common signs and symptoms may include:
- Persistent cough, sometimes with wheezing
- Shortness of breath or difficulty breathing
- Chest pain or discomfort
- Recurrent respiratory infections, such as pneumonia
- Fever of unknown origin
- General malaise, fatigue, and unexplained weight loss
- In some cases, a palpable mass in the chest or abdomen, though this is less common.
Due to the vague nature of these symptoms, a high index of suspicion is required, especially in young children with persistent or recurrent respiratory issues that do not respond to conventional treatments.
Treatment Approaches for Pleuropulmonary Blastoma
Effective pleuropulmonary blastoma treatment requires a multidisciplinary approach involving pediatric oncologists, surgeons, radiation oncologists, and pathologists. The specific treatment plan is highly individualized, depending on the tumor type, stage, size, and the child’s overall health. The primary goal is to remove the tumor completely and prevent recurrence.
The cornerstone of treatment for resectable tumors is surgical removal. Complete surgical resection, when feasible, offers the best chance for a cure, particularly for Type I tumors. For more advanced or aggressive tumors (Type II and III), surgery is often followed by adjuvant chemotherapy. Chemotherapy regimens typically include a combination of drugs designed to kill remaining cancer cells and reduce the risk of metastasis. Radiation therapy may also be considered in certain cases, especially for larger tumors or those that cannot be completely removed surgically, though its use is carefully weighed due to potential long-term side effects in growing children.
Ongoing research continues to explore new therapeutic strategies, including targeted therapies that specifically address the genetic mutations driving PPB, such as those involving the DICER1 gene. Long-term follow-up care, including regular imaging and clinical evaluations, is essential for monitoring for recurrence and managing any treatment-related complications. Families are often encouraged to participate in clinical trials to advance understanding and improve outcomes for children with this rare disease.