Key Takeaways
- Spinal cancer can be primary (originating in the spine) or secondary (metastasizing from elsewhere), with secondary tumors being more common.
- Common symptoms of spinal cancer include localized back pain, weakness, numbness, and bowel or bladder dysfunction.
- Spinal cancer diagnosis typically involves imaging studies like MRI, CT scans, and often a biopsy to confirm the tumor type.
- Spinal cancer treatment options range from surgery and radiation therapy to chemotherapy and targeted therapies, tailored to the individual case.
- The prognosis for spinal cancer varies widely depending on the tumor type, stage, and the patient’s overall health, emphasizing the importance of early intervention.
Understanding Spinal Cancer: Definition and Types
Spinal cancer encompasses a range of malignant tumors that develop in the spinal column or spinal cord. These tumors can disrupt the normal function of the nervous system, leading to a variety of symptoms. Understanding what is spinal cancer involves recognizing that these growths can originate directly in the spine or spread from other parts of the body.
Primary vs. Secondary Tumors
Spinal tumors are broadly categorized into two main types based on their origin:
- Primary Spinal Tumors: These tumors originate within the spinal column itself, including the vertebrae, spinal cord, or the surrounding membranes (meninges). Examples include gliomas, ependymomas, and meningiomas. While less common, these tumors can be benign or malignant.
- Secondary Spinal Tumors (Metastatic): Far more prevalent, these tumors develop when cancer cells from another part of the body (such as the lung, breast, prostate, or kidney) spread to the spine. The spine is a common site for metastasis due to its rich blood supply.
The specific types of spinal cancer are further classified by the cells from which they arise and their location within the spinal column:
| Location | Common Tumor Types | Characteristics |
|---|---|---|
| Intramedullary | Ependymomas, Astrocytomas | Grow within the spinal cord itself, often affecting nerve function directly. |
| Intradural-Extramedullary | Meningiomas, Nerve Sheath Tumors (Schwannomas, Neurofibromas) | Develop under the dura mater but outside the spinal cord, compressing it. |
| Extradural | Metastatic Tumors, Chordomas, Sarcomas | Occur outside the dura mater, often involving the vertebral bones. Most common type of spinal tumor. |
Potential Risk Factors
While the exact causes of spinal cancer are not always clear, certain factors may increase an individual’s risk. For primary spinal tumors, genetic syndromes play a role. For instance, neurofibromatosis type 2 (NF2) is linked to an increased risk of schwannomas and meningiomas, while von Hippel-Lindau disease is associated with hemangioblastomas. Exposure to certain chemicals or radiation therapy for other cancers might also contribute, though this is less definitively established for primary spinal tumors.
For secondary spinal tumors, the primary risk factor is having a pre-existing cancer elsewhere in the body, particularly those known to metastasize to bone, such as breast, lung, prostate, and kidney cancers. Age can also be a factor, as the incidence of cancer generally increases with age, thereby increasing the likelihood of metastatic spread to the spine.
Recognizing Symptoms of Spinal Tumors
The symptoms of spinal cancer can vary widely depending on the tumor’s location, size, and rate of growth. Early recognition is vital for timely intervention. These symptoms often arise from the tumor compressing the spinal cord, nerve roots, or affecting the stability of the spinal column.
Pain and Neurological Changes
Pain is the most common initial symptom, often localized to the back and sometimes radiating to other parts of the body. This pain may worsen at night or with activity and might not be relieved by rest or over-the-counter pain medications. As the tumor grows and compresses nerves or the spinal cord, neurological symptoms can develop:
- Weakness: Progressive weakness in the arms, legs, or both, which can lead to difficulty walking, stumbling, or dropping objects.
- Numbness or Sensory Loss: A loss of sensation, tingling, or “pins and needles” feeling in the extremities, often following a specific dermatomal pattern.
- Bowel or Bladder Dysfunction: In advanced stages or with significant spinal cord compression, individuals may experience incontinence or difficulty with urination or bowel movements. This is a medical emergency requiring immediate attention.
- Muscle Spasms: Involuntary muscle contractions or stiffness, particularly in the legs.
Other Systemic Signs
Beyond localized pain and neurological deficits, some individuals with spinal cancer, especially those with metastatic disease, may experience more general systemic symptoms. These can include unexplained weight loss, fatigue, fever, and night sweats. These non-specific symptoms are often indicative of advanced cancer elsewhere in the body that has spread to the spine. It is important to note that while these symptoms can be concerning, they can also be caused by many other less serious conditions. Persistent or worsening symptoms, especially neurological ones, warrant prompt medical evaluation.
Diagnosing Spinal Cancer Accurately
An accurate spinal cancer diagnosis is critical for determining the most effective treatment plan. The diagnostic process typically involves a combination of physical examination, neurological assessment, and advanced imaging techniques, often culminating in a biopsy.
Imaging and Biopsy Procedures
Imaging studies are fundamental in identifying the presence, location, and extent of a spinal tumor:
- Magnetic Resonance Imaging (MRI): This is the most common and detailed imaging test for spinal tumors. It provides high-resolution images of the spinal cord, nerve roots, and surrounding soft tissues, clearly showing the tumor’s size and relationship to vital structures. Contrast agents are often used to enhance visibility.
- Computed Tomography (CT) Scan: A CT scan provides detailed images of the bone structure of the spine, which is particularly useful for identifying bone destruction or instability caused by tumors. It can also be used in conjunction with a myelogram (CT myelography), where a contrast dye is injected into the spinal canal to highlight the spinal cord and nerve roots.
- Positron Emission Tomography (PET) Scan: Often used for metastatic spinal tumors, a PET scan can help identify the primary cancer site and detect other areas of cancer spread throughout the body.
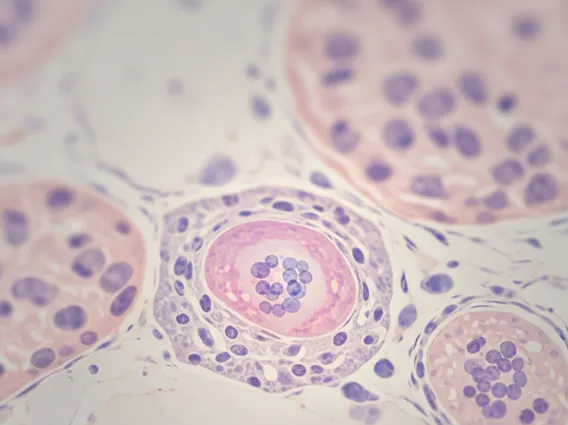
A definitive diagnosis of what is spinal cancer and its specific type usually requires a biopsy. During a biopsy, a small tissue sample from the tumor is removed and examined under a microscope by a pathologist. This procedure can be performed either through a needle biopsy (percutaneous, guided by imaging) or during open surgery, depending on the tumor’s location and accessibility.
Neurological Examination
A thorough neurological examination is an essential part of the diagnostic process. The physician will assess the patient’s reflexes, muscle strength, sensation, balance, and coordination. This helps to pinpoint which areas of the spinal cord or nerve roots are affected and provides crucial information about the extent of neurological impairment. Changes observed during the neurological exam can guide further imaging and help in planning treatment strategies.
Spinal Cancer Treatment Options
The choice of spinal cancer treatment options depends on several factors, including the type of tumor (primary or metastatic), its size and location, whether it’s benign or malignant, the patient’s overall health, and the extent of neurological deficits. A multidisciplinary team, often including neurosurgeons, oncologists, radiation oncologists, and rehabilitation specialists, typically collaborates to develop an individualized treatment plan.
Surgical and Radiation Therapies
Surgical intervention is often the primary treatment for many spinal tumors, especially those causing spinal cord compression. The goal of surgery is typically to remove as much of the tumor as safely possible while preserving neurological function and spinal stability. For benign tumors, complete surgical removal can often be curative. For malignant tumors, surgery aims to decompress the spinal cord and stabilize the spine, often followed by other therapies. Advances in surgical techniques, such as microsurgery and intraoperative monitoring, have improved outcomes and reduced risks.
Radiation therapy uses high-energy rays to destroy cancer cells and shrink tumors. It is a common treatment for both primary and metastatic spinal tumors, particularly when surgery is not feasible or when residual tumor remains after surgery. Techniques like conventional external beam radiation, stereotactic radiosurgery (SRS), and proton therapy allow for precise targeting of the tumor while minimizing damage to surrounding healthy tissues, including the delicate spinal cord. Radiation can help manage pain and prevent further neurological deterioration.
Systemic and Supportive Care
Systemic therapies, such as chemotherapy, targeted therapy, and immunotherapy, are often used for malignant spinal tumors, especially metastatic ones. Chemotherapy uses drugs to kill cancer cells throughout the body. Targeted therapies focus on specific molecules involved in cancer growth, while immunotherapy boosts the body’s immune system to fight cancer cells. These treatments are typically administered intravenously or orally and are chosen based on the specific type of cancer and its genetic profile.
Supportive care is an integral part of managing spinal cancer. This includes pain management, physical therapy to regain strength and mobility, occupational therapy to adapt to any functional limitations, and psychological support to help patients cope with the emotional challenges of their diagnosis and treatment. Corticosteroids may be used to reduce swelling around the spinal cord, providing temporary relief from compression symptoms. Rehabilitation plays a crucial role in improving quality of life and maximizing functional independence after treatment.
Prognosis and Long-Term Outlook
The prognosis for spinal cancer varies significantly among individuals, reflecting the diverse nature of these conditions. It is influenced by a multitude of factors, making it challenging to provide a generalized outlook. However, advancements in diagnostic tools and treatment modalities have steadily improved outcomes for many patients.
Factors Influencing Outcomes
Several key factors determine the long-term outlook for individuals diagnosed with spinal cancer:
- Tumor Type: Benign tumors generally have a better prognosis than malignant ones, especially if completely removable. Among malignant tumors, the specific histology (e.g., glioma vs. metastatic carcinoma) greatly impacts aggressiveness and response to treatment.
- Stage and Extent of Disease: For primary tumors, whether the cancer has spread beyond the spine is critical. For metastatic tumors, the type and extent of the primary cancer, as well as the number and location of other metastases, are crucial.
- Neurological Status at Diagnosis: Patients who present with minimal neurological deficits often have a better functional outcome after treatment compared to those with severe weakness or paralysis.
- Completeness of Resection: The ability to surgically remove the entire tumor (gross total resection) is a strong predictor of improved prognosis for many primary spinal tumors.
- Response to Treatment: How well the tumor responds to radiation, chemotherapy, or targeted therapies significantly impacts survival and recurrence rates.
- Overall Health and Age: Younger patients and those in good general health often tolerate aggressive treatments better and may have a more favorable prognosis.
According to the American Cancer Society, survival rates for spinal cord and brain tumors vary widely based on specific tumor types and patient demographics, underscoring the need for individualized assessment. Early diagnosis and prompt, aggressive treatment are consistently associated with better outcomes.
Life After Treatment
Life after treatment for spinal cancer often involves ongoing monitoring and rehabilitation. Regular follow-up appointments with imaging scans are essential to detect any recurrence or new tumor growth. Many patients will require physical therapy, occupational therapy, or other rehabilitative services to recover strength, mobility, and independence. Support groups and psychological counseling can also be invaluable resources for coping with the physical and emotional challenges. While the journey can be long, many individuals achieve a good quality of life following successful treatment, managing any residual symptoms and adapting to new routines. The focus remains on maximizing function and well-being.
No, spinal cancer is not always malignant. Spinal tumors can be either benign (non-cancerous) or malignant (cancerous). Benign tumors, such as meningiomas or schwannomas, grow slowly and typically do not spread, though they can still cause significant problems by compressing the spinal cord or nerves. Malignant tumors, including primary spinal cancers like ependymomas or metastatic cancers that spread to the spine, are more aggressive and have the potential to invade surrounding tissues or spread to other parts of the body. Accurate diagnosis through biopsy is essential to determine the tumor’s nature.
The progression of symptoms of spinal cancer varies widely depending on the tumor type, its growth rate, and its location. Some tumors, particularly benign ones, may grow slowly over months or even years, causing gradual onset of symptoms. More aggressive malignant tumors, especially metastatic ones, can cause rapid symptom progression over weeks or a few months, leading to quickly worsening pain, weakness, or neurological deficits. Sudden onset or rapid worsening of symptoms, especially neurological changes like severe weakness or bowel/bladder dysfunction, warrants immediate medical attention as it may indicate acute spinal cord compression.
The possibility of a cure for spinal cancer depends heavily on several factors, including whether the tumor is benign or malignant, its type, stage, and the extent to which it can be removed. Benign spinal tumors can often be cured with complete surgical resection. For malignant primary spinal cancers, a cure may be possible, especially with early diagnosis and aggressive multimodal treatment involving surgery, radiation, and sometimes chemotherapy. However, for metastatic spinal cancer, the goal of treatment is usually to control the disease, relieve symptoms, and improve quality of life, as a complete cure is often challenging due to the presence of cancer elsewhere in the body.