Transarterial Embolization
Transarterial embolization is a minimally invasive medical procedure used to block blood flow to specific areas, most commonly tumors or vascular malformations. This technique is a crucial option in interventional radiology, offering targeted treatment with reduced systemic impact.
Key Takeaways
- Transarterial Embolization (TAE) is a minimally invasive procedure that blocks blood supply to tumors or abnormal blood vessels.
- It involves inserting a catheter into an artery and delivering embolic agents to cut off blood flow to the target area.
- TAE is often used for liver cancers, providing a localized treatment option.
- Benefits include targeted therapy and reduced systemic side effects, while risks can involve pain, infection, or non-target embolization.
- Recovery typically involves a hospital stay of one to two days, with full recovery taking several weeks.
What is Transarterial Embolization?
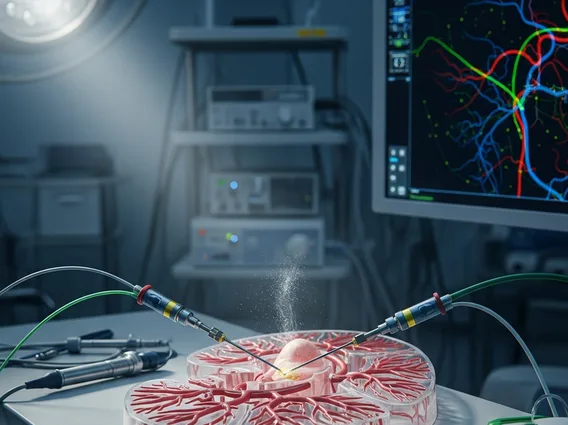
Transarterial Embolization (TAE) is a medical procedure that involves selectively blocking arteries to cut off the blood supply to a specific area, such as a tumor or an arteriovenous malformation. This technique is performed by interventional radiologists who use imaging guidance to navigate a catheter through the body’s arterial system to the target site. Once in position, embolic agents—which can be particles, coils, or liquid substances—are injected to occlude the blood vessels feeding the abnormal tissue.
The primary goal of what is transarterial embolization is to deprive the target tissue of oxygen and nutrients, leading to its shrinkage or destruction, while minimizing damage to surrounding healthy tissue. This approach is particularly effective for highly vascularized lesions, such as certain liver tumors, which rely heavily on arterial blood supply. For instance, hepatocellular carcinoma, a common form of liver cancer, often receives its primary blood supply from the hepatic artery, making it an ideal candidate for TAE. According to the World Health Organization (WHO), liver cancer remains a significant global health concern, and TAE plays an important role in its management.
Transarterial Embolization Procedure and Recovery
The transarterial embolization procedure typically begins with the patient receiving local anesthesia and often conscious sedation to ensure comfort. A small incision is made, usually in the groin, to access the femoral artery. A thin, flexible catheter is then inserted into the artery and carefully guided through the blood vessels using real-time X-ray imaging (fluoroscopy) until it reaches the arteries supplying the target area. Once the catheter is correctly positioned, the embolic agents are injected to block the blood flow. The specific type of embolic agent used depends on the condition being treated and the characteristics of the blood vessels.
Following the procedure, patients are monitored closely in a recovery area. The typical transarterial embolization recovery time involves a hospital stay of one to two days. During this period, patients may experience pain, nausea, or fever, which are usually managed with medication. Most individuals can resume light activities within a few days, but full recovery, including the resolution of fatigue and discomfort, can take several weeks. It is crucial for patients to follow their doctor’s post-procedure instructions carefully to ensure optimal healing and to monitor for any potential complications.
Key post-procedure care instructions often include:
- Avoiding strenuous activities and heavy lifting for at least one week.
- Keeping the incision site clean and dry to prevent infection.
- Taking prescribed pain medication as directed.
- Staying hydrated and maintaining a balanced diet.
- Reporting any severe pain, swelling, redness, or fever to the medical team immediately.
Benefits and Risks of Transarterial Embolization
The transarterial embolization benefits risks profile makes it a valuable treatment option for many patients. One of the primary benefits is its minimally invasive nature, which often results in less pain, shorter hospital stays, and quicker recovery compared to traditional open surgery. TAE provides highly targeted therapy, delivering embolic agents directly to the affected area, thereby minimizing systemic side effects and preserving healthy surrounding tissues. This precision is particularly advantageous for patients who may not be candidates for surgery due to other health conditions or the location of the lesion.
However, like any medical procedure, transarterial embolization carries potential risks. Common side effects include post-embolization syndrome, characterized by pain, fever, and nausea, which typically resolves within a few days. More serious, though less frequent, risks can include infection at the catheter insertion site, bleeding, damage to non-target organs or tissues due to unintended embolization, or allergic reactions to contrast dye. In rare cases, there can be complications such as liver abscesses or kidney dysfunction, especially in patients with pre-existing conditions. A thorough discussion with a healthcare provider about individual risks and benefits is essential before undergoing the procedure.
