Programmed Cell Death
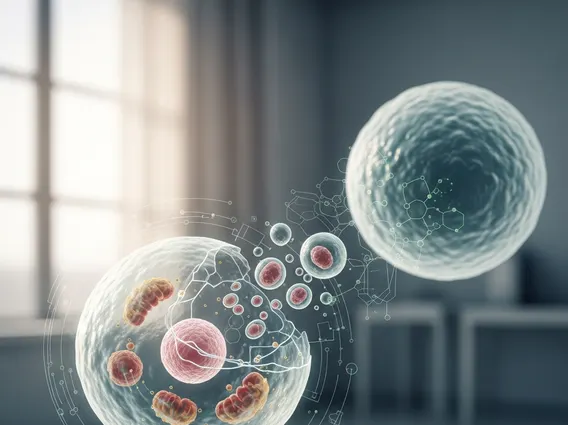
Programmed Cell Death (PCD) is a fundamental biological process essential for the development, maintenance, and health of multicellular organisms. It involves a series of tightly regulated cellular events that lead to the elimination of cells in a controlled manner.
Key Takeaways
- Programmed Cell Death is a vital, genetically controlled process for removing unwanted or damaged cells.
- It plays crucial roles in embryonic development, tissue homeostasis, and defense against disease.
- The primary forms include apoptosis, necroptosis, and autophagy, each with distinct molecular mechanisms.
- Dysregulation of PCD can contribute to various diseases, including cancer and neurodegenerative disorders.
What is Programmed Cell Death?
Programmed Cell Death refers to a highly regulated and genetically controlled process by which cells are eliminated from an organism. Unlike necrosis, which is uncontrolled cell death resulting from acute injury, PCD is an active process that serves critical physiological functions. The programmed cell death definition encompasses its role in maintaining tissue homeostasis, shaping organs during development, and removing potentially harmful cells, such as those infected by viruses or those with DNA damage that could lead to cancer.
This intricate cellular mechanism is vital for the proper functioning and survival of an organism. For instance, during embryonic development, PCD is responsible for sculpting tissues and organs, such as the removal of webbing between fingers and toes. In adults, it continuously eliminates old, damaged, or superfluous cells, ensuring the balance between cell proliferation and cell death. The precise control over this process is paramount, as both insufficient and excessive PCD can have severe pathological consequences.
Types of Programmed Cell Death
There are several distinct types of programmed cell death, each characterized by unique morphological features and molecular pathways. The most well-known and extensively studied type is apoptosis, but others like necroptosis and autophagy also play significant roles in various biological contexts.
- Apoptosis: Often referred to as “cellular suicide,” apoptosis is a highly regulated process where cells shrink, condense their chromatin, and fragment into apoptotic bodies. These bodies are then efficiently engulfed by phagocytes, preventing inflammation. It is crucial for development, immune system regulation, and tumor suppression.
- Necroptosis: This is a form of regulated necrosis that shares some features with apoptosis but is typically initiated when apoptotic pathways are inhibited. Necroptosis is highly inflammatory, as it involves cell swelling and rupture, releasing cellular contents into the extracellular space. It plays a role in host defense against certain pathogens and in inflammatory diseases.
- Autophagy: While primarily a cellular recycling process that degrades and recycles cellular components, autophagy can also lead to cell death under specific conditions. Autophagy-dependent cell death is characterized by the accumulation of autophagosomes and autolysosomes, and it is distinct from apoptosis and necroptosis in its morphological features.
Understanding these different types is crucial for deciphering their roles in health and disease, as their dysregulation can contribute to conditions ranging from neurodegeneration to autoimmune disorders.
How Programmed Cell Death Works
The intricate mechanisms of how programmed cell death works involve a complex interplay of molecular signals and effector proteins. For apoptosis, the process is primarily mediated by a family of proteases called caspases, which are activated in a cascade-like manner. There are two main pathways leading to caspase activation: the extrinsic (death receptor) pathway and the intrinsic (mitochondrial) pathway.
The extrinsic pathway is triggered by external signals, such as the binding of death ligands (e.g., Fas ligand, TNF-alpha) to specific death receptors on the cell surface. This binding leads to the formation of a death-inducing signaling complex (DISC), which activates initiator caspases (e.g., caspase-8). The intrinsic pathway, on the other hand, is activated by internal cellular stress, such as DNA damage, growth factor withdrawal, or endoplasmic reticulum stress. This pathway involves the permeabilization of the outer mitochondrial membrane, leading to the release of pro-apoptotic factors like cytochrome c into the cytoplasm. Cytochrome c then binds to Apaf-1, forming an apoptosome that activates initiator caspases (e.g., caspase-9).
Both pathways converge on the activation of executioner caspases (e.g., caspase-3, -6, -7), which are responsible for cleaving various cellular substrates, leading to the characteristic morphological changes of apoptosis, such as DNA fragmentation, cytoskeletal breakdown, and cell shrinkage. The final stage involves the recognition and engulfment of apoptotic cells by phagocytes, ensuring the orderly removal of cellular debris without inducing inflammation.
Note: The information provided in this article is for educational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.



















