Plexiform Neurofibroma
Plexiform Neurofibroma is a complex, benign tumor that arises from nerve sheaths and is a hallmark feature of Neurofibromatosis Type 1 (NF1). These tumors can grow extensively, affecting various parts of the body and potentially causing significant health challenges.

Key Takeaways
- Plexiform Neurofibroma is a non-cancerous tumor associated with Neurofibromatosis Type 1 (NF1).
- It can cause disfigurement, pain, and functional impairment due to its invasive growth pattern.
- Symptoms vary widely depending on the tumor’s size and location, ranging from visible lumps to internal organ compression.
- The primary cause is a genetic mutation in the NF1 gene, which plays a crucial role in cell growth regulation.
- Treatment options include surgical removal, targeted drug therapies, and supportive care, often requiring a multidisciplinary approach.
What is Plexiform Neurofibroma?
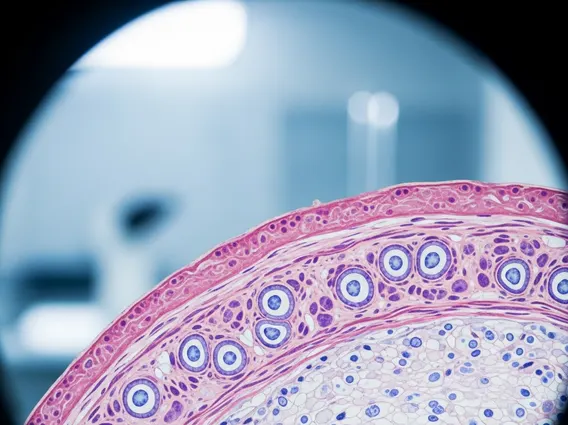
Plexiform Neurofibroma refers to a type of benign nerve sheath tumor that is characterized by its diffuse, infiltrative growth pattern along multiple nerve bundles. Unlike cutaneous neurofibromas, which are typically small and superficial, plexiform neurofibromas can grow very large and deep, often involving multiple tissue layers, including skin, subcutaneous tissue, muscle, and even bone. These tumors are almost exclusively associated with Neurofibromatosis Type 1 (NF1), a genetic disorder affecting approximately 1 in 3,000 live births worldwide, according to the National Institute of Neurological Disorders and Stroke (NINDS).
While generally non-cancerous, plexiform neurofibromas can cause significant morbidity due to their potential for disfigurement, pain, and functional impairment. They can also undergo malignant transformation into malignant peripheral nerve sheath tumors (MPNSTs) in a small percentage of cases, typically around 8-13% over a lifetime, making regular monitoring crucial for affected individuals.
Identifying Plexiform Neurofibroma: Symptoms and Causes
The presentation of plexiform neurofibroma symptoms can vary widely depending on the tumor’s size, location, and depth. These symptoms often develop during childhood and can progress over time. Common signs include:
- Visible or palpable soft tissue masses, which may feel like a “bag of worms” under the skin.
- Pain or tenderness in the affected area, often due to nerve compression or stretching.
- Disfigurement, especially when tumors affect the face or limbs, leading to asymmetry or overgrowth of tissues.
- Neurological deficits such as weakness, numbness, or tingling if the tumor compresses major nerves.
- Functional impairment, affecting movement, vision, or breathing, depending on the tumor’s proximity to vital organs or joints.
- Internal complications, such as bladder dysfunction, bowel obstruction, or spinal cord compression, when tumors grow internally.
The underlying causes of plexiform neurofibroma are rooted in genetics. These tumors arise from a mutation in the NF1 gene, located on chromosome 17. This gene codes for a protein called neurofibromin, which acts as a tumor suppressor. When the NF1 gene is mutated, neurofibromin function is impaired, leading to uncontrolled cell growth and proliferation of Schwann cells, fibroblasts, and mast cells, which are the primary components of these tumors. Most cases of NF1 are inherited from a parent, but approximately 30-50% arise from spontaneous new mutations.
Plexiform Neurofibroma Treatment Options
Managing plexiform neurofibroma treatment options typically involves a multidisciplinary approach, tailored to the individual patient’s specific needs, tumor characteristics, and symptom burden. Given the complex nature of these tumors, treatment strategies aim to alleviate symptoms, prevent complications, and improve quality of life.
Surgical resection is often the primary treatment for accessible tumors causing significant symptoms or functional impairment. However, complete surgical removal can be challenging due to the infiltrative nature of plexiform neurofibromas and their close association with vital nerves and blood vessels. Surgeons often aim for debulking, removing as much of the tumor as safely possible to reduce mass effect and pain. Advances in surgical techniques, including microsurgery, have improved outcomes, but recurrence is common.
In recent years, targeted drug therapies have emerged as a significant advancement. MEK inhibitors, such as selumetinib, have shown promise in shrinking plexiform neurofibromas and improving associated symptoms in children with NF1. These medications work by blocking a specific signaling pathway involved in cell growth, offering a non-surgical option for managing tumor progression. Radiation therapy is generally less commonly used due to the risk of malignant transformation and potential long-term side effects, but it may be considered in select cases, particularly for malignant peripheral nerve sheath tumors.