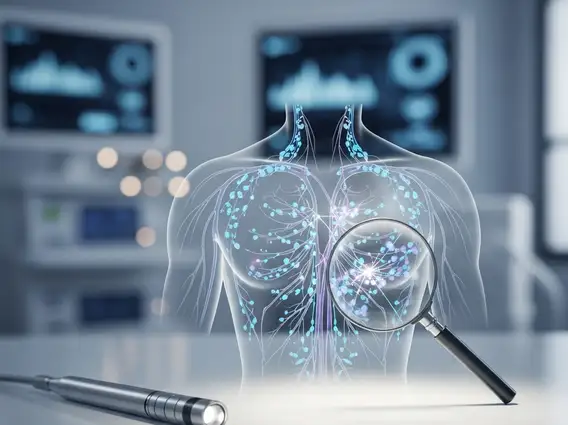
Lymphatic Mapping
Lymphatic Mapping is a crucial diagnostic technique used in oncology to identify the primary lymph nodes that drain a tumor site. This procedure helps guide treatment decisions, particularly in various types of cancer, by determining the potential spread of cancer cells.
Key Takeaways
- Lymphatic Mapping identifies the sentinel lymph node(s), the first lymph nodes to which cancer cells are most likely to spread from a primary tumor.
- The procedure involves injecting a tracer (dye, radioisotope, or both) near the tumor to visualize the lymphatic pathways.
- It is primarily used in cancer staging, especially for melanoma and breast cancer, to assess regional lymph node involvement.
- By accurately identifying affected nodes, Lymphatic Mapping helps avoid unnecessary extensive lymph node dissections, reducing patient morbidity.
- The technique significantly impacts treatment planning, guiding surgical approaches and adjuvant therapies.
What is Lymphatic Mapping?
Lymphatic Mapping refers to a specialized medical procedure designed to locate the sentinel lymph node(s) (SLN) that drain a specific area of the body, typically a tumor site. The purpose of lymphatic mapping is to identify these first-draining lymph nodes, as they are the most likely to contain metastatic cancer cells if the disease has begun to spread. This technique is invaluable for accurately staging cancer and guiding subsequent treatment strategies, allowing for more targeted interventions.
By pinpointing the sentinel node, clinicians can determine whether cancer has spread beyond the primary tumor without needing to remove a large number of lymph nodes. This precision helps in making informed decisions about the extent of surgical intervention required and whether additional therapies, such as radiation or chemotherapy, are necessary. The procedure has revolutionized the management of several cancers by minimizing the invasiveness of treatment while maintaining diagnostic accuracy.
The Lymphatic Mapping Procedure
The lymphatic mapping procedure explained involves several key steps to visualize the lymphatic drainage pathways from a tumor. The process typically begins with the injection of a tracer substance near the primary tumor site. This tracer can be a blue dye, a radioactive isotope, or a combination of both, which then travels through the lymphatic vessels to the first lymph nodes in the drainage basin.
Here’s how lymphatic mapping works:
- Tracer Injection: A small amount of blue dye (e.g., isosulfan blue or methylene blue) or a radioactive tracer (e.g., technetium-99m sulfur colloid) is injected around the tumor.
- Migration: The tracer is absorbed by the lymphatic system and travels along the lymphatic vessels, following the natural drainage path.
- Detection: For radioactive tracers, a gamma probe (a handheld device that detects radioactivity) is used externally over the skin to locate the “hot spot” where the tracer has accumulated in the sentinel node(s). For blue dye, the surgeon visually identifies the stained lymph node(s) during surgery.
- Excision and Biopsy: Once identified, the sentinel lymph node(s) are surgically removed and sent for pathological examination to check for the presence of cancer cells.
This method allows for the removal of only the most relevant lymph nodes, reducing the risk of complications associated with extensive lymph node dissection, such as lymphedema.
Clinical Applications of Lymphatic Mapping
Lymphatic Mapping has become a standard of care in the management of several types of cancer, significantly improving patient outcomes and quality of life. Its primary application is in determining the regional spread of cancer, which is a critical factor in staging the disease and planning appropriate treatment.
The most common clinical applications include:
- Melanoma: For patients with intermediate-thickness melanoma, Lymphatic Mapping helps identify if cancer cells have spread to regional lymph nodes, guiding decisions on further lymph node dissection or adjuvant therapy.
- Breast Cancer: In early-stage breast cancer, sentinel lymph node biopsy (SLNB) performed after Lymphatic Mapping has largely replaced axillary lymph node dissection for many patients, reducing the incidence of lymphedema. According to the American Cancer Society, SLNB is successful in identifying the sentinel node in over 90% of cases for breast cancer and melanoma, providing accurate staging information with less morbidity.
- Other Cancers: While less common, Lymphatic Mapping is also explored and utilized in certain cases of colorectal cancer, gynecological cancers (e.g., cervical, endometrial, vulvar), and head and neck cancers to assess regional lymph node involvement.
By precisely identifying the sentinel node, this technique allows for personalized treatment plans, minimizing unnecessary surgical interventions and their associated risks, while ensuring that patients receive effective therapy for their specific cancer stage.