Esophagogastroduodenoscopy
Esophagogastroduodenoscopy, commonly known as EGD, is a diagnostic and therapeutic procedure used to examine the upper part of the gastrointestinal tract. This procedure allows healthcare providers to visualize the esophagus, stomach, and duodenum to identify and address various conditions.
Key Takeaways
- Esophagogastroduodenoscopy (EGD) is a procedure to visually inspect the esophagus, stomach, and duodenum.
- Its primary purpose is to diagnose and treat conditions affecting the upper digestive system, such as ulcers, inflammation, and bleeding.
- Preparation typically involves fasting and adjusting certain medications to ensure clear visualization and patient safety.
- Recovery is usually brief, with patients monitored until sedation wears off, and they should arrange for transportation home.
- EGD is a safe and effective method for investigating symptoms like persistent heartburn, difficulty swallowing, or unexplained abdominal pain.
What is Esophagogastroduodenoscopy (EGD) and Its Purpose?
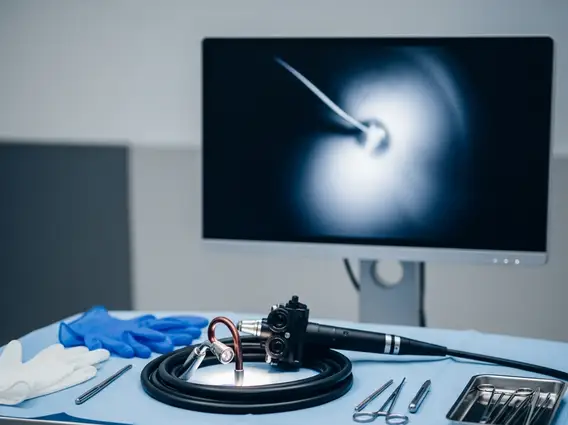
Esophagogastroduodenoscopy (EGD) is a comprehensive EGD medical procedure explanation for examining the upper gastrointestinal (GI) tract. This diagnostic and therapeutic technique involves the use of an endoscope—a thin, flexible tube equipped with a light and camera—which is gently guided through the mouth, down the esophagus, into the stomach, and finally into the duodenum. The camera transmits real-time images to a monitor, allowing the physician to meticulously inspect the lining of these organs for abnormalities.
The primary purpose of esophagogastroduodenoscopy is multifaceted, encompassing both diagnostic evaluation and therapeutic intervention. Diagnostically, it helps identify the causes of symptoms such as persistent heartburn, difficulty swallowing, unexplained abdominal pain, nausea, vomiting, or gastrointestinal bleeding. For instance, it can detect conditions like ulcers, inflammation (esophagitis, gastritis), celiac disease, and even early signs of cancer. Therapeutically, the procedure allows for the removal of polyps, dilation of narrowed areas, or stopping active bleeding using specialized instruments passed through the endoscope. The Centers for Disease Control and Prevention (CDC) highlights endoscopy as a vital tool in the early detection and management of gastrointestinal diseases, significantly improving patient outcomes.
Common reasons a physician might recommend an EGD include:
- Investigating the cause of persistent upper abdominal pain, nausea, vomiting, or difficulty swallowing.
- Diagnosing and evaluating conditions such as gastroesophageal reflux disease (GERD), ulcers, inflammation, or celiac disease.
- Screening for and monitoring precancerous conditions or early cancers in the esophagus, stomach, or duodenum.
- Treating certain conditions, such as removing polyps, dilating strictures, or controlling bleeding.
Esophagogastroduodenoscopy (EGD) Preparation and Recovery
Proper Esophagogastroduodenoscopy preparation and recovery are essential for the safety and effectiveness of the procedure. Preparation typically begins several days before the EGD. Patients are usually instructed to fast for a specific period, often 6-8 hours, before the procedure, meaning no food or drink. This ensures the stomach is empty, allowing for clear visualization and reducing the risk of aspiration. Additionally, patients may need to adjust certain medications, particularly blood thinners or diabetes medications, under the guidance of their physician to prevent complications.
On the day of the procedure, an intravenous (IV) line will be placed to administer a sedative, helping the patient relax and remain comfortable. The procedure itself usually takes 15-30 minutes. After the EGD, patients are moved to a recovery area where they are monitored as the sedation wears off. It is common to experience a sore throat, bloating, or mild cramping, which typically subside quickly. Due to the effects of sedation, patients are not permitted to drive and must arrange for someone to transport them home. Most individuals can resume their normal diet and activities the following day, though specific post-procedure instructions will be provided by the healthcare team.



















