Endoscopic Ultrasound Guided Fine Needle Aspiration
Endoscopic Ultrasound Guided Fine Needle Aspiration (EUS-FNA) is a sophisticated medical procedure that plays a crucial role in diagnosing various conditions affecting the gastrointestinal tract and surrounding organs. This minimally invasive technique allows physicians to obtain tissue samples for accurate pathological examination.
Key Takeaways
- EUS-FNA is a minimally invasive procedure used for diagnosing conditions in the GI tract and adjacent organs.
- It combines endoscopy with ultrasound imaging to precisely target and sample suspicious lesions.
- The procedure involves inserting an endoscope with an ultrasound probe, guiding a fine needle to the target, and aspirating cells or tissue.
- Key benefits include high diagnostic accuracy, reduced invasiveness compared to surgery, and the ability to access hard-to-reach areas.
- EUS-FNA is vital for staging cancers and diagnosing benign conditions, aiding in personalized treatment plans.
What is Endoscopic Ultrasound Guided Fine Needle Aspiration (EUS-FNA)?
Endoscopic Ultrasound Guided Fine Needle Aspiration (EUS-FNA) refers to a diagnostic procedure that combines endoscopy and ultrasound technology to obtain tissue samples from internal organs. This technique is primarily used to evaluate abnormalities within or adjacent to the gastrointestinal (GI) tract, such as lesions in the pancreas, bile ducts, liver, lymph nodes, and the walls of the esophagus, stomach, and duodenum. The procedure provides a detailed eus guided fine needle aspiration explanation of suspicious masses or fluid collections by allowing direct visualization and sampling. It is considered a highly effective method for diagnosing various conditions, including cancers, infections, and inflammatory diseases, without the need for more invasive surgical interventions.
The EUS-Guided FNA Procedure Explained
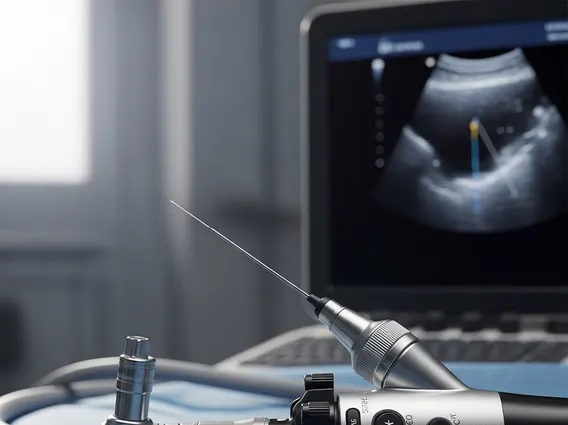
The endoscopic ultrasound guided fna procedure involves several key steps, typically performed in an outpatient setting under sedation. Patients are usually given a sedative to ensure comfort throughout the procedure. An endoscope, which is a thin, flexible tube equipped with a camera and an ultrasound transducer at its tip, is gently inserted into the patient’s mouth and guided through the esophagus, stomach, and into the duodenum. The ultrasound component generates detailed images of the organs and surrounding structures, allowing the physician to precisely locate and visualize the target lesion.
Once the target is identified, a very fine needle is passed through a channel in the endoscope and advanced into the suspicious area under real-time ultrasound guidance. Cells or fluid are then aspirated into the needle. Multiple passes may be performed to ensure an adequate sample is collected. The collected tissue is immediately sent to a pathology laboratory for microscopic examination. The entire procedure typically takes between 30 to 90 minutes, depending on the complexity and location of the lesion.
- Preparation: Patients fast for several hours prior to the procedure.
- Sedation: Intravenous sedation is administered for comfort.
- Endoscope Insertion: A specialized endoscope is advanced to the area of interest.
- Ultrasound Imaging: Real-time ultrasound identifies the target lesion.
- Needle Aspiration: A fine needle is guided to the lesion to collect samples.
- Sample Analysis: Collected samples are sent for pathological examination.
Benefits of Endoscopic Ultrasound Aspiration
The benefits of endoscopic ultrasound aspiration are significant, making it a preferred diagnostic tool in many clinical scenarios. One of its primary advantages is its high diagnostic accuracy, particularly for pancreatic lesions and mediastinal lymph nodes. Studies have shown EUS-FNA to have a diagnostic accuracy ranging from 85% to 95% for pancreatic masses, as reported by institutions like the American Society for Gastrointestinal Endoscopy (ASGE). This precision allows for earlier and more accurate diagnosis, which is critical for timely treatment planning, especially in oncology.
Furthermore, EUS-FNA is a minimally invasive procedure, meaning it involves smaller incisions or no incisions at all, leading to less pain, fewer complications, and a faster recovery time compared to traditional surgical biopsies. It also provides access to areas that are difficult to reach with other imaging or biopsy techniques, such as lesions deep within the abdomen or chest. By providing definitive tissue diagnoses, EUS-FNA helps clinicians differentiate between benign and malignant conditions, guiding appropriate management strategies and potentially avoiding unnecessary surgeries. This diagnostic capability is invaluable for staging cancers, assessing tumor resectability, and monitoring disease progression.