Key Takeaways
- Salivary gland cancer is uncommon, accounting for a small percentage of all head and neck cancers.
- Symptoms often include a painless lump in the jaw, neck, or mouth, or facial numbness.
- Diagnosis typically involves a physical exam, imaging, and a definitive biopsy.
- Treatment primarily consists of surgery, often followed by radiation therapy.
- The salivary gland cancer prognosis varies significantly based on the cancer’s type, stage, and location.
Salivary Gland Cancer: An Overview
What is Salivary Gland Cancer?
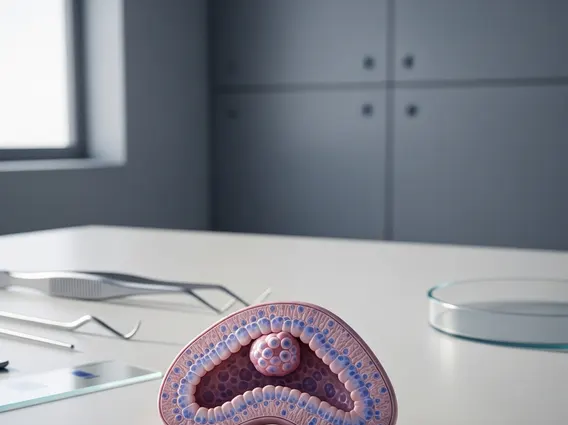
The salivary glands are exocrine glands that produce saliva, essential for moistening food, initiating digestion, and protecting teeth from decay. There are three major pairs of salivary glands—the parotid, submandibular, and sublingual glands—and hundreds of minor salivary glands located throughout the mouth and throat. What is salivary gland cancer? It is a malignant growth that develops in these glands, most commonly in the parotid glands. This type of cancer is relatively rare; according to the American Cancer Society, it represents less than 1% of all cancers and approximately 6% of all head and neck cancers in the United States. While many tumors in the salivary glands are benign, a definitive diagnosis through biopsy is critical to determine their nature.
Common Types of Salivary Gland Cancer
The classification of types of salivary gland cancer is complex due to the diverse cell types present in the glands. These cancers are categorized based on their cellular origin and microscopic appearance. Understanding the specific type is vital as it influences treatment strategies and prognosis.
Some of the most common malignant types include:
- Mucoepidermoid Carcinoma: This is the most prevalent type, often arising in the parotid glands. It can range from low-grade (slow-growing, less aggressive) to high-grade (fast-growing, more aggressive).
- Adenoid Cystic Carcinoma: Known for its tendency to spread along nerves (perineural invasion) and its potential for distant metastasis, even years after initial treatment. It can occur in any salivary gland but is common in minor salivary glands.
- Adenocarcinoma: A broad category that includes several subtypes, such as polymorphous adenocarcinoma and salivary duct carcinoma. These can vary widely in aggressiveness and location.
- Acinic Cell Carcinoma: Typically a low-grade cancer, it often affects the parotid gland and has a relatively good prognosis, though it can recur locally.
- Malignant Mixed Tumor (Carcinoma Ex Pleomorphic Adenoma): This occurs when a pre-existing benign pleomorphic adenoma transforms into a malignant tumor. This transformation is more likely in long-standing benign tumors.
Recognizing Symptoms
Early Signs and Manifestations
The symptoms of salivary gland cancer can be subtle in their early stages, often mimicking less serious conditions. However, recognizing persistent or worsening signs is crucial for timely medical evaluation. The most common initial symptom is the presence of a lump or swelling.
Key symptoms to be aware of include:
- Painless Lump or Swelling: A persistent lump or swelling in or near the ear, cheek, jaw, or neck is the most frequent symptom. While often painless, any new or growing mass should be investigated.
- Facial Numbness or Weakness: As the tumor grows, it can affect nearby nerves, leading to numbness, tingling, or weakness in parts of the face. This can manifest as difficulty moving one side of the face.
- Persistent Pain: While early lumps are often painless, localized pain in the salivary gland area, jaw, or neck that does not subside can be a sign of advanced disease.
- Difficulty Swallowing (Dysphagia): If the tumor is located in a gland near the throat, it can interfere with the swallowing process.
- Trouble Opening the Mouth Widely (Trismus): A tumor affecting the muscles or nerves around the jaw can restrict jaw movement.
- Fluid Drainage from the Ear: In rare cases, a tumor in the parotid gland might cause fluid or pus to drain from the ear.
It is important to note that many of these symptoms can also be caused by non-cancerous conditions, such as infections or benign tumors. However, any persistent or concerning symptom warrants prompt consultation with a healthcare professional for proper diagnosis.
Causes and Risk Factors
Identifying Potential Risks
The exact causes of salivary gland cancer are not fully understood, and in many cases, the disease develops without any identifiable risk factors. However, research has identified several factors that may increase an individual’s likelihood of developing this rare cancer.
Potential risk factors include:
- Radiation Exposure: A history of radiation therapy to the head and neck, particularly for other cancers, is a well-established risk factor. Exposure to high doses of radiation from environmental sources, such as nuclear accidents, has also been linked to an increased risk.
- Age: The risk of developing salivary gland cancer generally increases with age, with most diagnoses occurring in individuals over 50.
- Occupational Exposures: Some studies suggest a possible link between certain occupational exposures and an elevated risk. This includes working with specific types of dust (e.g., silica dust) or in industries involving rubber manufacturing or asbestos. However, more research is needed to establish definitive links.
- Certain Viral Infections: While less direct than for other head and neck cancers, some viruses, such as the Epstein-Barr virus (EBV) and human papillomavirus (HPV), are being studied for their potential role in a small subset of salivary gland cancers.
- Genetic Syndromes: Very rarely, certain inherited genetic syndromes, such as Li-Fraumeni syndrome, may increase the risk of various cancers, including salivary gland cancer.
It is crucial to remember that having one or more risk factors does not guarantee that an individual will develop salivary gland cancer, and many people who develop the disease have no known risk factors.
Diagnosing Salivary Gland Cancer
Diagnostic Procedures
The diagnosis of salivary gland cancer involves a series of steps to accurately identify the presence, type, and extent of the cancer. A thorough diagnostic process is essential for planning effective treatment.
The typical diagnostic procedures include:
- Physical Examination: A doctor will carefully examine the head and neck area, feeling for any lumps, swelling, or signs of facial nerve weakness. They will also assess the patient’s medical history and symptoms.
- Imaging Tests: Various imaging techniques are used to visualize the salivary glands and surrounding structures, helping to determine the size, location, and potential spread of a tumor.
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images, useful for assessing bone involvement and lymph node status.
- Magnetic Resonance Imaging (MRI): Offers excellent soft tissue contrast, making it ideal for evaluating the tumor’s relationship to nerves and blood vessels.
- Positron Emission Tomography (PET) Scan: Often combined with CT (PET-CT), it helps identify metabolically active cancer cells throughout the body, useful for detecting distant metastasis.
- Biopsy: This is the definitive diagnostic procedure. A small sample of tissue from the suspicious area is removed and examined under a microscope by a pathologist to confirm the presence of cancer cells and determine the specific type of cancer.
- Fine Needle Aspiration (FNA) Biopsy: A thin needle is used to extract cells from the lump. It is less invasive but may not always provide enough tissue for a definitive diagnosis of all tumor types.
- Incisional or Excisional Biopsy: If FNA is inconclusive or more tissue is needed, a small incision may be made to remove part (incisional) or all (excisional) of the tumor.
- Staging: Once cancer is confirmed, further tests may be conducted to determine the stage of the cancer, which describes its size, whether it has spread to nearby lymph nodes, and if it has metastasized to distant parts of the body. This information is critical for guiding treatment decisions.
Treatment Approaches and Prognosis
Available Treatment Options
The treatment for salivary gland cancer is highly individualized, depending on the type, stage, location of the tumor, and the patient’s overall health. A multidisciplinary team, including surgeons, radiation oncologists, and medical oncologists, typically collaborates to develop the most effective treatment plan.
Primary treatment modalities include:
- Surgery: This is the cornerstone of treatment for most salivary gland cancers. The goal is to remove the tumor along with a margin of healthy tissue. The extent of surgery depends on the tumor’s size and location. For parotid gland tumors, a parotidectomy is performed. In some cases, nearby lymph nodes may also be removed (neck dissection) if there is a risk of cancer spread.
- Radiation Therapy: Often used after surgery (adjuvant therapy) to destroy any remaining cancer cells and reduce the risk of recurrence, especially for high-grade tumors, those with positive margins, or those that have spread to lymph nodes. It can also be used as the primary treatment for patients who are not candidates for surgery or for advanced, unresectable tumors.
- Chemotherapy: This is generally less effective for salivary gland cancers compared to other cancer types. It is typically reserved for advanced cancers that have spread to distant sites (metastatic disease) or for recurrent cancers that cannot be treated with surgery or radiation.
- Targeted Therapy: These drugs specifically target certain molecules involved in cancer growth and spread. While research is ongoing, some targeted therapies may be used for specific subtypes of salivary gland cancer that have particular genetic mutations.
Rehabilitation, including physical therapy and speech therapy, may be necessary after treatment, especially if facial nerves or swallowing functions are affected.
Understanding the Outlook
The salivary gland cancer prognosis varies significantly among individuals, influenced by several critical factors. These include the specific type of cancer, its grade (how aggressive it appears under a microscope), the stage at which it is diagnosed (size, lymph node involvement, distant spread), the tumor’s location, and the patient’s overall health and response to treatment.
Generally, smaller, low-grade tumors detected early tend to have a more favorable prognosis. For instance, according to data from the National Cancer Institute, the 5-year survival rate for localized salivary gland cancer can be over 90%, while for distant metastatic disease, it can be considerably lower. Cancers arising in the major salivary glands (like the parotid) often have a better outlook than those in the minor salivary glands, which can be more aggressive. Adenoid cystic carcinoma, while often slow-growing, has a propensity for late recurrence and distant metastasis, which can affect long-term survival rates. Regular follow-up care is essential for monitoring for recurrence and managing any long-term side effects of treatment, playing a crucial role in the overall outlook.
No, a lump in a salivary gland is not always cancerous. In fact, the majority of salivary gland tumors are benign (non-cancerous). Common benign conditions include pleomorphic adenomas and Warthin’s tumors. However, because it is impossible to distinguish between benign and malignant lumps based on symptoms alone, any new or persistent lump in the salivary gland area should be promptly evaluated by a healthcare professional. A biopsy is typically required to definitively determine if the lump is cancerous.
Yes, salivary gland cancer can spread, or metastasize, to other parts of the body. The primary routes of spread are to nearby lymph nodes in the neck and, less commonly, to distant organs such as the lungs, bones, or liver. The likelihood of spread depends on the specific type and stage of the cancer. High-grade tumors and certain aggressive types like adenoid cystic carcinoma have a higher propensity for metastasis. Regular follow-up and imaging are crucial to monitor for any signs of local recurrence or distant spread.
Recovery after treatment for salivary gland cancer, particularly surgery, varies depending on the extent of the procedure and the gland involved. Patients may experience pain, swelling, and temporary numbness in the surgical area. If the facial nerve is near the tumor, there’s a risk of temporary or, rarely, permanent facial weakness or paralysis. Rehabilitation, including physical therapy, may be necessary to restore function. Most patients can return to normal activities within a few weeks, but ongoing monitoring and follow-up appointments are essential for long-term recovery and cancer surveillance.