Key Takeaways
- Nasopharyngeal Cancer is a malignancy originating in the nasopharynx, more common in specific geographic regions like Southeast Asia.
- Early signs nasopharyngeal cancer can be subtle, including persistent ear problems, nasal blockage, or a neck lump, often leading to delayed diagnosis.
- The Epstein-Barr Virus (EBV) is a primary cause of nasopharyngeal cancer, alongside genetic predisposition and environmental factors like diet and smoking.
- Nasopharyngeal cancer diagnosis involves a combination of endoscopy, biopsy, and advanced imaging techniques to confirm the disease and determine its stage.
- Treatment for nasopharyngeal cancer primarily includes radiation therapy and chemotherapy, with a generally favorable nasopharyngeal cancer prognosis when detected early.
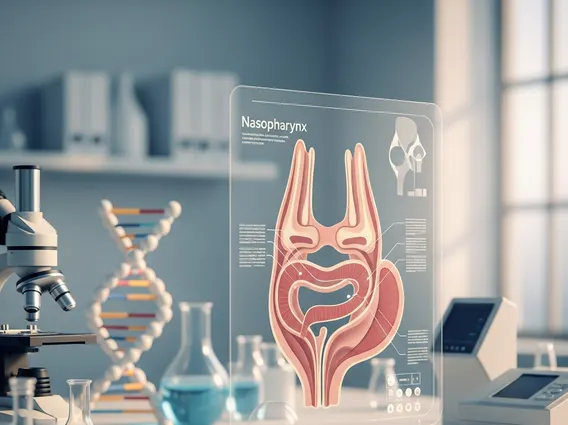
What is Nasopharyngeal Cancer?
Nasopharyngeal Cancer is a malignant tumor that develops in the nasopharynx, the area located behind the nose and above the back of the throat. This region serves as a passageway for air from the nose to the lungs. Unlike many other head and neck cancers, NPC is relatively uncommon in Western countries but shows a significantly higher incidence in certain parts of Asia, particularly southern China and Southeast Asia, as well as North Africa and the Arctic regions. According to the American Cancer Society, NPC accounts for less than 1% of all cancers in the United States but is one of the most common cancers in some endemic areas.
Understanding NPC Development
The development of Nasopharyngeal Cancer typically begins when cells in the nasopharynx undergo genetic mutations, leading to uncontrolled growth and the formation of a tumor. These cells are usually squamous cells, which line the surface of the nasopharynx. The cancer can then spread locally to surrounding structures or metastasize to distant parts of the body through the lymphatic system or bloodstream. Its hidden location makes early detection challenging, as tumors can grow considerably before causing noticeable symptoms.
Types of Nasopharyngeal Carcinoma
There are three main histological types of nasopharyngeal carcinoma, classified by the World Health Organization (WHO):
- Type I: Keratinizing Squamous Cell Carcinoma: This type is less common and is not strongly associated with the Epstein-Barr virus. It typically affects older individuals and has a prognosis similar to other head and neck squamous cell carcinomas.
- Type II: Non-keratinizing Carcinoma (Differentiated): This type is intermediate in prevalence and shows some association with EBV.
- Type III: Undifferentiated Carcinoma (Non-keratinizing, Undifferentiated): This is the most common type, especially in endemic regions, and is strongly linked to the Epstein-Barr virus. It is often highly sensitive to radiation therapy.
The classification helps guide treatment strategies and provides insight into the likely underlying causes and biological behavior of the tumor.
Recognizing Nasopharyngeal Cancer Symptoms
Recognizing nasopharyngeal cancer symptoms can be challenging because they are often non-specific and can mimic those of less serious conditions, leading to delays in diagnosis. Awareness of these signs is crucial for prompt medical evaluation.
Early Warning Signs of NPC
The early signs nasopharyngeal cancer are often subtle and can include symptoms affecting the ears, nose, and neck. These symptoms may persist or worsen over time:
- Ear Problems: Persistent unilateral hearing loss, a feeling of fullness in one ear, or recurrent ear infections, often due to the tumor blocking the Eustachian tube. Tinnitus (ringing in the ear) can also be an early indicator.
- Nasal Symptoms: Chronic nasal blockage or stuffiness, especially on one side, that does not resolve with conventional treatments. Frequent nosebleeds (epistaxis) or blood-tinged discharge from the nose can also occur.
- Neck Lump: The most common initial symptom is often a painless lump or swelling in the neck, typically due to enlarged lymph nodes where cancer cells have spread. This lump is usually firm and non-tender.
- Sore Throat or Hoarseness: Persistent throat discomfort or changes in voice quality, though less common as an initial symptom.
Advanced Symptoms and Complications
As the disease progresses, nasopharyngeal cancer symptoms can become more pronounced and indicative of local or distant spread:
- Headaches: Persistent or severe headaches, particularly if they are new or worsening, can indicate tumor extension into the skull base.
- Facial Numbness or Pain: Involvement of cranial nerves can lead to numbness, tingling, or pain in the face, often affecting one side.
- Double Vision (Diplopia): If the tumor affects nerves controlling eye movement, patients may experience double vision or difficulty moving their eyes.
- Difficulty Swallowing or Speaking: Advanced tumors can impair the function of the throat, leading to dysphagia (difficulty swallowing) or dysarthria (difficulty speaking).
- Weight Loss and Fatigue: Unexplained weight loss, loss of appetite, and persistent fatigue are general symptoms of advanced cancer.
Causes and Risk Factors for NPC
Understanding the causes of nasopharyngeal cancer involves examining a combination of viral, environmental, and genetic factors that contribute to its development. While the exact interplay is complex, several key risk factors have been identified.
Viral Connections (EBV)
The most significant and consistent risk factor for Nasopharyngeal Cancer, particularly the undifferentiated type prevalent in endemic regions, is infection with the Epstein-Barr Virus (EBV). EBV is a common human herpesvirus that infects most people worldwide, often causing no symptoms or mild illness like infectious mononucleosis. However, in certain individuals and specific genetic contexts, chronic EBV infection can lead to cellular changes that promote cancer development in the nasopharynx. The presence of EBV DNA and proteins is consistently found in NPC tumor cells, highlighting its critical role in the disease’s etiology.
Environmental and Genetic Influences
Beyond EBV, several other factors contribute to the risk of developing NPC:
- Dietary Factors: A diet high in traditionally preserved foods, such as salted fish and fermented vegetables, particularly during childhood, is strongly linked to NPC in high-incidence areas. These foods contain nitrosamines, which are known carcinogens.
- Genetics: Individuals with a family history of NPC have an increased risk, suggesting a genetic predisposition. Specific genetic markers and variations in human leukocyte antigen (HLA) genes have been associated with susceptibility to the disease.
- Smoking and Alcohol: While less strongly linked than for other head and neck cancers, heavy smoking and alcohol consumption are considered risk factors for NPC, especially for the keratinizing squamous cell carcinoma type.
- Occupational Exposure: Exposure to certain industrial chemicals, such as wood dust or formaldehyde, has been suggested as a potential risk factor, though this link is less definitive.
It is the combination of these factors, particularly EBV infection in genetically susceptible individuals exposed to specific environmental triggers, that significantly increases the likelihood of developing Nasopharyngeal Cancer.
Diagnosis of Nasopharyngeal Cancer
A timely and accurate nasopharyngeal cancer diagnosis is critical for effective treatment planning and improving patient outcomes. The diagnostic process typically involves a series of physical examinations, specialized tests, and imaging studies.
Diagnostic Procedures and Tests
When a patient presents with suspicious symptoms, a thorough diagnostic workup is initiated:
- Physical Examination: The doctor will examine the head and neck, feeling for any lumps in the neck and checking for facial asymmetry or cranial nerve deficits.
- Nasopharyngoscopy: This is a key procedure where a thin, flexible tube with a light and camera (endoscope) is inserted through the nose to visualize the nasopharynx directly. This allows the doctor to identify any abnormal growths or lesions.
- Biopsy: If a suspicious area is found during nasopharyngoscopy, a tissue sample (biopsy) is taken. This is the definitive test for diagnosing cancer. The tissue is then examined under a microscope by a pathologist to confirm the presence of cancer cells and determine the specific type of NPC.
- Imaging Tests:
- MRI (Magnetic Resonance Imaging): Often used to assess the extent of the tumor in the nasopharynx and its spread to nearby structures, such as the skull base or brain.
- CT (Computed Tomography) Scan: Provides detailed images of the head and neck, and sometimes the chest and abdomen, to check for distant spread.
- PET (Positron Emission Tomography) Scan: Often combined with a CT scan (PET-CT), this scan helps identify metabolically active cancer cells throughout the body, detecting both the primary tumor and any metastatic sites.
- Blood Tests: Blood tests, including a complete blood count and liver/kidney function tests, are performed to assess overall health. In endemic areas, tests for EBV DNA in the blood can also be used as a diagnostic marker and for monitoring treatment response.
Staging the Cancer
Once cancer is confirmed, staging is performed to determine the extent of the disease. Staging is crucial for guiding treatment for nasopharyngeal cancer and predicting nasopharyngeal cancer prognosis. The most common system used is the TNM (Tumor, Node, Metastasis) system:
- T (Tumor): Describes the size and extent of the primary tumor.
- N (Nodes): Indicates whether cancer has spread to nearby lymph nodes and, if so, their size, number, and location.
- M (Metastasis): Denotes whether cancer has spread to distant parts of the body (e.g., bones, lungs, liver).
Based on these factors, NPC is assigned a stage from 0 to IV, with higher stages indicating more advanced disease. This comprehensive evaluation ensures that patients receive the most appropriate and effective treatment plan.
Treatment Options and Outlook
The treatment for nasopharyngeal cancer is highly individualized, depending on the cancer’s stage, the patient’s overall health, and other specific factors. Due to its location and radiosensitivity, radiation therapy is often the cornerstone of treatment.
Common Treatment Approaches
The primary treatment modalities for NPC include:
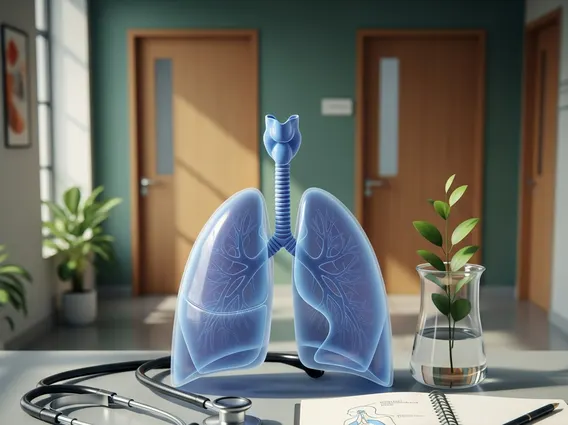
- Radiation Therapy: This is the main treatment for most stages of NPC. High-energy X-rays or other particles are used to kill cancer cells or keep them from growing. Advanced techniques like Intensity-Modulated Radiation Therapy (IMRT) precisely target the tumor while sparing surrounding healthy tissues, reducing side effects.
- Chemotherapy: Often used in conjunction with radiation therapy (concurrent chemoradiation) for locally advanced disease, chemotherapy drugs help kill cancer cells throughout the body. It can also be given before radiation (induction chemotherapy) to shrink the tumor or after treatment (adjuvant chemotherapy) to eliminate any remaining cancer cells. For metastatic disease, chemotherapy is the primary systemic treatment.
- Targeted Therapy: These drugs target specific molecules involved in cancer growth and spread, offering a more precise approach with potentially fewer side effects than traditional chemotherapy. Examples include epidermal growth factor receptor (EGFR) inhibitors.
- Immunotherapy: This treatment harnesses the body’s immune system to fight cancer. Immune checkpoint inhibitors, for instance, block proteins that prevent the immune system from attacking cancer cells, allowing the immune system to recognize and destroy them.
- Surgery: Surgery is rarely the primary treatment for the initial tumor due to the nasopharynx’s complex anatomical location. However, it may be considered for recurrent disease or to remove affected lymph nodes in the neck after other treatments.
Prognosis and Follow-up Care
The nasopharyngeal cancer prognosis varies significantly depending on several factors, including the stage at diagnosis, the specific type of NPC, the patient’s overall health, and their response to treatment. Generally, NPC has a relatively favorable prognosis compared to other head and neck cancers, especially when diagnosed at an early stage. For localized disease, the 5-year survival rate can be quite high. However, prognosis worsens with regional or distant spread.
After completing treatment, regular follow-up care is essential. This typically involves frequent physical examinations, blood tests (including EBV DNA levels), and imaging scans (MRI, CT, PET) to monitor for recurrence or new primary tumors. Long-term follow-up also addresses potential late side effects of treatment, such as dry mouth, hearing changes, or thyroid dysfunction, ensuring comprehensive care and maintaining quality of life.
Nasopharyngeal Cancer is relatively rare globally, accounting for less than 1% of all cancers in many Western countries. However, its prevalence is significantly higher in specific geographic regions. It is endemic in Southern China, Southeast Asia, and parts of North Africa, where it is one of the most common cancers. For instance, in some parts of China, the incidence can be as high as 20-50 cases per 100,000 people per year, compared to less than 1 case per 100,000 in most Western populations, highlighting a distinct geographical distribution.
While complete prevention of Nasopharyngeal Cancer is challenging due to its complex etiology, certain measures can reduce risk. Avoiding excessive consumption of salted and preserved foods, especially during childhood, is recommended in high-risk areas. Quitting smoking and reducing alcohol intake can also lower the risk, particularly for certain types of NPC. Research into an Epstein-Barr Virus (EBV) vaccine is ongoing, which could potentially offer a significant preventive strategy given EBV’s strong association with the disease.
The recovery process after treatment for nasopharyngeal cancer can be extensive, often involving managing side effects from radiation and chemotherapy. Patients may experience dry mouth (xerostomia), difficulty swallowing, hearing changes, fatigue, and skin irritation. Rehabilitation, including physical therapy, speech therapy, and nutritional counseling, is often crucial to help patients regain function and manage long-term side effects. Regular follow-up appointments are vital for monitoring recovery, detecting any recurrence, and addressing ongoing health concerns to ensure the best possible quality of life.