Key Takeaways
- Endometrial Cancer begins in the lining of the uterus and is the most common gynecologic cancer.
- Abnormal vaginal bleeding, especially after menopause, is the most common and critical symptom.
- Risk factors include hormonal imbalances (excess estrogen), obesity, diabetes, and certain genetic conditions.
- Diagnosis typically involves a biopsy of the uterine lining, followed by staging to determine the extent of the cancer.
- Treatment often includes surgery (hysterectomy) and may be followed by radiation, chemotherapy, or hormone therapy, depending on the stage and type.
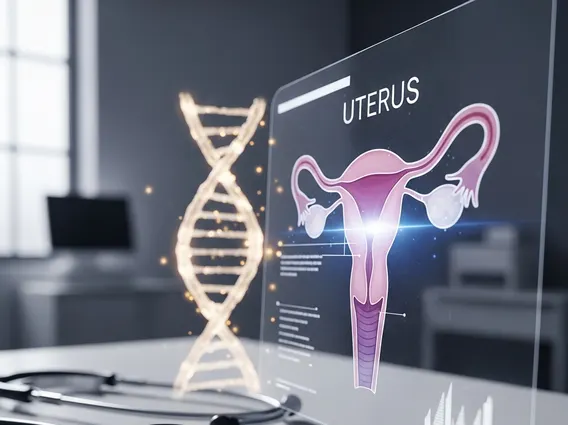
What is Endometrial Cancer?
What is endometrial cancer? It is a malignancy that develops from the cells lining the uterus, called the endometrium. This cancer typically grows slowly and is often detected at an early stage due to its common symptom of abnormal vaginal bleeding. According to the American Cancer Society, an estimated 66,200 new cases of uterine body cancers (primarily endometrial cancers) are diagnosed in the U.S. each year, with approximately 13,030 deaths. It is more prevalent in postmenopausal women, with the average age of diagnosis being 60 years old.
Types of Endometrial Cancer
Endometrial cancer is broadly categorized into two main types:
- Type 1 (Estrogen-dependent): This is the most common type, accounting for about 80-90% of cases. It is often linked to excess estrogen exposure and typically presents as endometrioid adenocarcinoma. These cancers are generally less aggressive, grow slowly, and are often diagnosed at an early stage.
- Type 2 (Non-estrogen-dependent): This type is less common but tends to be more aggressive. It includes serous carcinoma, clear cell carcinoma, and carcinosarcoma. These cancers are not strongly associated with estrogen and are more likely to spread outside the uterus, often diagnosed at a more advanced stage.
How it Develops
Endometrial cancer develops when cells in the endometrium begin to grow abnormally and uncontrollably, forming a tumor. This process often starts with a condition called endometrial hyperplasia, where the lining becomes too thick due to an imbalance of hormones, particularly excess estrogen without sufficient progesterone. While hyperplasia is not cancer, certain types, especially atypical hyperplasia, can be a precursor to cancer. Over time, these abnormal cells can acquire mutations that lead to malignant transformation, allowing them to invade surrounding tissues and potentially spread to other parts of the body.
Key Symptoms of Endometrial Cancer
Recognizing endometrial cancer symptoms early is crucial for effective treatment. The most common symptom is abnormal vaginal bleeding, which should always prompt medical evaluation, especially in postmenopausal women.
Common Warning Signs
The primary warning signs of endometrial cancer are related to changes in vaginal bleeding patterns:
- Postmenopausal Bleeding: Any vaginal bleeding, spotting, or discharge after menopause is the most common and significant symptom, occurring in about 90% of cases.
- Abnormal Vaginal Bleeding in Younger Women: This can include unusually heavy or prolonged menstrual periods (menorrhagia), bleeding between periods, or any irregular bleeding that is not typical for an individual’s cycle.
- Pelvic Pain or Pressure: Some women may experience pain, cramping, or a feeling of pressure in the lower abdomen or pelvis, particularly as the tumor grows larger.
- Unusual Vaginal Discharge: A watery, blood-tinged, or foul-smelling discharge that is not blood may also be a symptom.
- Changes in Bowel or Bladder Habits: In advanced stages, if the tumor presses on nearby organs, it can cause changes such as difficulty urinating, painful urination, or constipation.
When to See a Doctor
It is imperative to consult a doctor immediately if you experience any abnormal vaginal bleeding, particularly if you are postmenopausal. While these symptoms can be caused by conditions other than cancer, prompt evaluation is essential to rule out endometrial cancer or diagnose it at its earliest, most treatable stage. Do not delay seeking medical advice for any persistent or unusual gynecological symptoms.
Risk Factors for Endometrial Cancer
Understanding the endometrial cancer risk factors can help individuals and healthcare providers assess personal risk and consider preventive strategies. Many factors influencing the causes of endometrial cancer are related to hormonal balance and lifestyle.
Hormonal Influences
The primary driver for many endometrial cancers is prolonged exposure to estrogen without sufficient progesterone to balance its effects. This can occur due to:
- Obesity: Fat tissue can convert other hormones into estrogen, leading to higher estrogen levels. This is a significant risk factor, with obese women having a 3-4 times higher risk than women of healthy weight.
- Estrogen-only Hormone Therapy: Taking estrogen without progesterone after menopause increases risk. Combined hormone therapy (estrogen and progesterone) does not carry the same risk.
- Early Menstruation and Late Menopause: A longer lifetime exposure to estrogen due to starting periods early or going through menopause late increases risk.
- Never Having Been Pregnant (Nulliparity): Pregnancy temporarily reduces estrogen exposure, so women who have never been pregnant have a slightly higher risk.
- Tamoxifen Use: This drug, used in breast cancer treatment, can act like estrogen in the uterus, increasing risk.
- Polycystic Ovary Syndrome (PCOS): This condition can lead to higher estrogen levels and lower progesterone levels.
Lifestyle and Genetic Factors
Beyond hormonal influences, other factors contribute to the risk profile:
- Age: The risk of endometrial cancer increases significantly with age, with most diagnoses occurring in women over 50.
- Diabetes: Women with type 2 diabetes have an increased risk, possibly due to insulin resistance and its effects on hormone levels.
- Diet High in Animal Fat: Some studies suggest a link between diets high in animal fats and increased risk.
- Genetic Syndromes: Certain inherited conditions significantly increase risk. The most notable is Lynch syndrome (also known as hereditary non-polyposis colorectal cancer or HNPCC), which accounts for 2-5% of all endometrial cancers.
Diagnosis and Staging
Accurate endometrial cancer diagnosis and staging are critical steps to determine the extent of the disease and plan the most effective treatment strategy. A series of procedures are typically involved to confirm the presence of cancer and assess its spread.
Diagnostic Procedures
If endometrial cancer symptoms are present, a doctor will perform several diagnostic tests:
- Pelvic Exam: A physical examination to check for any abnormalities in the uterus, ovaries, and vagina.
- Transvaginal Ultrasound (TVUS): An imaging test that uses sound waves to create pictures of the uterus and ovaries, allowing the doctor to measure the thickness of the endometrium and look for masses.
- Endometrial Biopsy: This is the primary diagnostic tool. A thin, flexible tube is inserted through the cervix into the uterus to collect a small tissue sample from the endometrium. This sample is then examined under a microscope for cancer cells.
- Dilation and Curettage (D&C): If an endometrial biopsy is inconclusive or insufficient, a D&C may be performed. This procedure involves dilating the cervix and gently scraping tissue from the uterine lining for pathological examination.
- Hysteroscopy: A thin, lighted tube with a camera is inserted into the uterus to visualize the endometrium directly and take targeted biopsies.
- Imaging Tests: If cancer is confirmed, imaging tests like MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans of the abdomen and pelvis may be used to look for signs of cancer spread to other organs or lymph nodes.
Understanding Cancer Stages
The stages of endometrial cancer describe how far the cancer has spread. Staging is typically determined during surgery, as it allows for direct visualization and biopsy of potentially affected areas. The most common staging system is the FIGO (International Federation of Gynecology and Obstetrics) system:
| Stage | Description |
|---|---|
| Stage I | Cancer is confined to the uterus. |
| Stage II | Cancer has spread to the cervix but has not extended beyond the uterus. |
| Stage III | Cancer has spread outside the uterus to nearby structures such as the ovaries, fallopian tubes, vagina, or nearby lymph nodes, but not to distant organs. |
| Stage IV | Cancer has spread to distant organs, such as the bladder, bowel, lungs, liver, or bones. |
Staging is crucial for guiding endometrial cancer treatment options and predicting prognosis.
Endometrial Cancer Treatment Options
The choice of endometrial cancer treatment options depends on several factors, including the stage and type of cancer, the patient’s overall health, and personal preferences. Treatment plans are often multidisciplinary, involving gynecologic oncologists, radiation oncologists, and medical oncologists.
Surgical Interventions
Surgery is the primary treatment for most cases of endometrial cancer, especially in early stages. The main surgical procedures include:
- Total Hysterectomy: This involves the removal of the entire uterus, including the cervix. It can be performed abdominally, laparoscopically, or robotically.
- Bilateral Salpingo-Oophorectomy (BSO): The fallopian tubes and ovaries are typically removed at the same time as the hysterectomy, as these are common sites for cancer spread.
- Lymph Node Dissection: Lymph nodes in the pelvis and sometimes around the aorta are often removed to check for cancer spread. This helps in accurate staging and guides further treatment.
- Radical Hysterectomy: In some cases, particularly if the cancer has spread to the cervix, a more extensive surgery that removes the uterus, cervix, part of the vagina, and surrounding tissues may be necessary.
Adjuvant Therapies
After surgery, or in cases of advanced or recurrent cancer, additional treatments known as adjuvant therapies may be recommended to destroy any remaining cancer cells and reduce the risk of recurrence:
- Radiation Therapy: This uses high-energy rays to kill cancer cells. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy), where radioactive sources are placed directly into the vagina or uterus.
- Chemotherapy: This involves using drugs, given intravenously or orally, to kill cancer cells throughout the body. It is typically used for more advanced stages of cancer or when cancer has recurred.
- Hormone Therapy: For hormone-sensitive cancers (primarily Type 1), high doses of progesterone may be used to slow or stop cancer growth. This is sometimes an option for women who wish to preserve fertility in very early-stage, low-grade cancers.
- Targeted Therapy and Immunotherapy: These newer treatments focus on specific molecular targets in cancer cells or boost the body’s immune system to fight cancer. They are typically reserved for advanced or recurrent cases that have not responded to standard treatments.
While endometrial cancer cannot be entirely prevented, certain measures can significantly reduce the risk. Maintaining a healthy weight through diet and exercise is crucial, as obesity is a major risk factor. Managing conditions like diabetes and discussing the risks and benefits of hormone replacement therapy with your doctor are also important. Promptly reporting any abnormal vaginal bleeding, especially after menopause, allows for early detection, which is key to successful treatment.
The prognosis for endometrial cancer is generally favorable, especially when diagnosed at an early stage. For localized disease (Stage I), the 5-year survival rate is very high, often exceeding 90%. Prognosis depends on the cancer’s stage, type, grade, and the patient’s overall health. Early detection through awareness of endometrial cancer symptoms and timely medical intervention significantly improves outcomes and the effectiveness of endometrial cancer treatment options.
Women who are postmenopausal are at the highest risk for endometrial cancer, with the average age of diagnosis around 60. Key endometrial cancer risk factors include obesity, which leads to increased estrogen levels, and type 2 diabetes. Other factors include never having been pregnant, early onset of menstruation, late menopause, and certain genetic conditions like Lynch syndrome. Women with these risk factors should be particularly vigilant about symptoms and discuss screening with their healthcare providers.