Parietal Cell Vagotomy
Parietal Cell Vagotomy is a surgical procedure primarily used to treat peptic ulcer disease by reducing the stomach’s acid production. This highly selective operation aims to alleviate symptoms and promote healing while minimizing potential side effects.
Key Takeaways
- Parietal Cell Vagotomy is a targeted surgical intervention for peptic ulcers, reducing gastric acid secretion.
- The procedure selectively severs nerve branches supplying acid-producing parietal cells, leaving other stomach functions intact.
- Its primary purpose is to decrease acid production, promoting ulcer healing and preventing recurrence.
- Compared to older vagotomy techniques, it aims for fewer digestive side effects.
- Potential complications, though generally less severe, can include delayed gastric emptying or recurrent ulcers.
What is Parietal Cell Vagotomy?
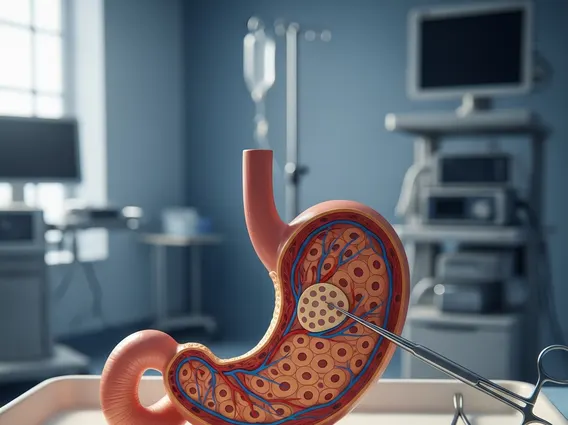
Parietal Cell Vagotomy refers to a highly selective surgical procedure designed to reduce the stomach’s capacity to produce acid. This operation targets the vagus nerve branches that specifically innervate the parietal cells, which are responsible for secreting hydrochloric acid in the stomach. By selectively cutting these nerve fibers, the procedure significantly diminishes acid output without affecting the innervation of other parts of the stomach, such as the antrum or pylorus, which control gastric motility.
This surgical approach was developed as an advancement over earlier, less selective vagotomy techniques. Its precision aims to preserve normal stomach emptying and reduce the incidence of post-surgical complications often associated with more extensive nerve transections. It is primarily considered for patients suffering from chronic or recurrent peptic ulcers that have not responded to conventional medical therapies.
Parietal Cell Vagotomy: Procedure and Purpose
The parietal cell vagotomy procedure explained involves carefully identifying and severing only the small nerve branches of the vagus nerve that supply the acid-secreting parietal cells in the fundus and body of the stomach. The main trunks of the vagus nerve and the nerve fibers controlling the antrum (the lower part of the stomach) and pylorus (the outlet valve) are preserved. This preservation is crucial because these nerves regulate stomach emptying, and their disruption can lead to significant digestive issues.
The purpose of parietal cell vagotomy is fundamentally to decrease the production of gastric acid, thereby creating an environment conducive to the healing of peptic ulcers and preventing their recurrence. By reducing acid secretion, the corrosive effect on the stomach or duodenal lining is mitigated. This procedure is particularly effective for duodenal ulcers, which are often exacerbated by excessive acid. The selective nature of the surgery means that patients typically experience fewer post-operative complications related to gastric motility compared to those undergoing truncal or selective vagotomy.
The procedure can be performed through an open incision (laparotomy) or, more commonly today, using minimally invasive laparoscopic techniques. Laparoscopic surgery generally results in less pain, smaller scars, and a faster recovery time for the patient.
Potential Side Effects of Parietal Cell Vagotomy
While parietal cell vagotomy side effects are generally less severe and less frequent than those associated with older, less selective vagotomy procedures, they can still occur. The primary goal of this selective approach is to avoid complications like dumping syndrome or delayed gastric emptying, which are common after truncal vagotomy.
Potential side effects may include:
- Recurrent Ulceration: Despite the reduction in acid, some patients may still experience a recurrence of peptic ulcers, though this is less common than with medical management alone.
- Delayed Gastric Emptying (Gastroparesis): Although the nerves to the pylorus are preserved, some patients may still experience a temporary or, rarely, persistent delay in stomach emptying, leading to symptoms like nausea, vomiting, and bloating.
- Diarrhea: While less common than with truncal vagotomy, some patients may experience changes in bowel habits.
- Heartburn or Reflux: Changes in stomach function can sometimes exacerbate or induce symptoms of gastroesophageal reflux disease (GERD).
According to a review of surgical outcomes, the incidence of recurrent ulceration after parietal cell vagotomy is reported to be between 5-10%, which is significantly lower than the recurrence rates observed with medical therapy alone for some ulcer types (Source: American College of Surgeons Clinical Congress reports, general surgical literature). Patients considering this surgery should discuss these potential risks and benefits thoroughly with their healthcare provider.