Ovarian Transposition
Ovarian transposition is a surgical procedure designed to move a woman’s ovaries out of a planned radiation field. This intervention aims to protect ovarian function and preserve fertility for patients undergoing treatments that could otherwise damage these vital reproductive organs.

Key Takeaways
- Ovarian transposition is a surgical technique to relocate ovaries, primarily to shield them from radiation damage during cancer treatment.
- The procedure helps preserve a woman’s fertility and hormonal function.
- It typically involves minimally invasive laparoscopic surgery, moving the ovaries to a safer location within the abdomen.
- Benefits include the potential to conceive naturally or through assisted reproductive technologies and avoiding premature menopause.
- Potential risks include surgical complications, pain, and the possibility of ovarian failure despite the procedure.
What is Ovarian Transposition?
Ovarian Transposition is a medical procedure involving the surgical relocation of the ovaries from their natural position in the pelvis to another site in the abdomen, typically higher up and away from the pelvic region. The primary purpose of this technique is to protect the ovaries from the damaging effects of radiation therapy, which is often used to treat pelvic cancers such as cervical, rectal, or bladder cancer. By moving the ovaries outside the anticipated radiation field, the procedure significantly reduces the risk of radiation-induced ovarian failure, thereby preserving a woman’s ability to produce hormones and potentially conceive in the future. According to the American Cancer Society, approximately 70,000 adolescents and young adults (ages 15-39) are diagnosed with cancer each year in the United States, many of whom are of reproductive age. For those requiring pelvic radiation, preserving ovarian function becomes a critical concern, highlighting the importance of procedures like ovarian transposition.
The Ovarian Transposition Procedure
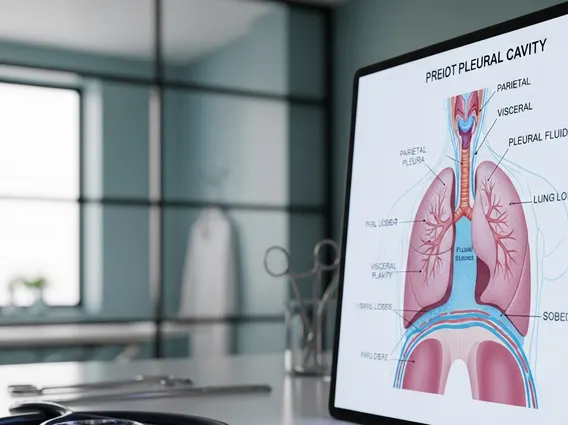
The ovarian transposition procedure is typically performed using minimally invasive laparoscopic techniques, though an open surgical approach may be necessary in certain cases. During a laparoscopic procedure, a surgeon makes several small incisions in the abdomen, through which a laparoscope (a thin, lighted tube with a camera) and specialized surgical instruments are inserted. The ovaries, along with their blood supply, are carefully dissected from their original attachments in the pelvis. They are then meticulously repositioned to a new location, often in the upper abdomen or flanks, ensuring they are outside the planned radiation treatment area. The new position is secured by suturing the ovaries to the abdominal wall or surrounding tissues, maintaining their blood supply to ensure viability. This careful relocation is crucial for minimizing radiation exposure while preserving the ovaries’ ability to function.
Benefits and Potential Side Effects of Ovarian Transposition
The primary benefits of ovarian transposition are centered on preserving a woman’s reproductive and endocrine health. By shielding the ovaries from radiation, the procedure significantly reduces the risk of premature ovarian insufficiency and early menopause. This allows women to maintain natural hormone production, which is vital for bone health, cardiovascular well-being, and overall quality of life. Furthermore, it preserves the potential for future fertility, giving patients the option to conceive naturally or through assisted reproductive technologies after cancer treatment. This can be a significant psychological benefit for young women facing cancer diagnoses.
However, like any surgical intervention, there are potential ovarian transposition side effects. These can include general surgical risks such as bleeding, infection, and damage to surrounding organs. Specific to ovarian transposition, patients may experience chronic pelvic pain or the formation of adhesions, which are bands of scar tissue that can cause discomfort or complications. There is also a risk that the transposed ovaries may not function optimally despite being moved, leading to ovarian failure or reduced hormone production. In rare instances, the ovaries might migrate back into the radiation field, or their blood supply could be compromised during the relocation, affecting their viability. Patients should discuss these potential risks and benefits thoroughly with their healthcare team to make informed decisions about their treatment plan.