Oophorectomy
Oophorectomy is a surgical procedure involving the removal of one or both ovaries. This operation is performed for various medical reasons, ranging from treating diseases to reducing cancer risk.
Key Takeaways
- Oophorectomy is the surgical removal of one or both ovaries.
- It can be performed to treat conditions like ovarian cysts, endometriosis, or cancer, and as a preventive measure.
- The procedure can be unilateral (one ovary) or bilateral (both ovaries), and often involves minimally invasive or open surgical techniques.
- Potential risks include bleeding, infection, damage to surrounding organs, and menopausal symptoms if both ovaries are removed.
- Recovery time varies, typically involving a few weeks for full activity resumption, with post-surgery care focusing on pain management and monitoring for complications.
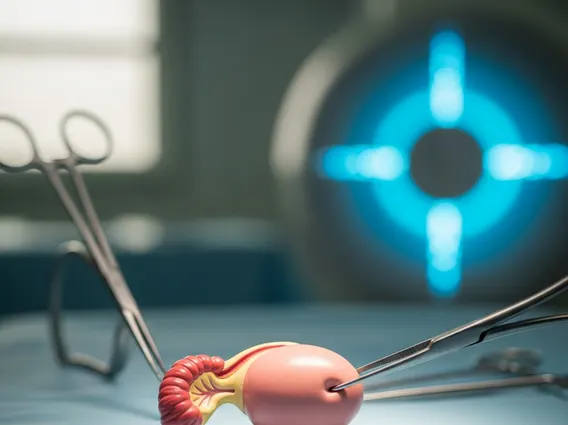
What is Oophorectomy?
Oophorectomy refers to the surgical removal of one or both ovaries. The ovaries are female reproductive glands located in the pelvis that produce eggs and female hormones (estrogen and progesterone). This procedure can be performed for a variety of medical indications, making it a significant intervention in women’s health. Understanding what is Oophorectomy involves recognizing its different forms and purposes.
There are several types of oophorectomy. A unilateral oophorectomy involves removing only one ovary, while a bilateral oophorectomy involves removing both ovaries. When the fallopian tube on the same side is also removed, the procedure is called a salpingo-oophorectomy. If both ovaries and both fallopian tubes are removed, it’s a bilateral salpingo-oophorectomy. The decision to perform an oophorectomy is typically made after careful consideration of the patient’s age, medical history, and specific condition. Common reasons include treating ovarian cysts, endometriosis, pelvic inflammatory disease, or ovarian cancer. It can also be a prophylactic measure to reduce the risk of ovarian cancer in individuals with a high genetic predisposition, such as those with BRCA gene mutations.
Oophorectomy Procedure: Steps and Potential Risks
The oophorectomy procedure details vary depending on the surgical approach chosen by the surgeon. The two primary methods are laparoscopic surgery (minimally invasive) and open abdominal surgery.
- Laparoscopic Oophorectomy: This is often preferred due to its less invasive nature. The surgeon makes several small incisions in the abdomen. A laparoscope, a thin tube with a camera, is inserted through one incision to visualize the pelvic organs. Surgical instruments are then inserted through other incisions to carefully detach and remove the ovary or ovaries. This method typically results in less pain, smaller scars, and a quicker recovery compared to open surgery.
- Open Oophorectomy: This involves a single, larger incision in the lower abdomen, similar to a C-section incision. This approach provides the surgeon with a direct view of the pelvic organs and may be necessary for larger ovarian masses, extensive disease, or in cases where laparoscopic surgery is not feasible.
Like any surgical intervention, there are risks of oophorectomy surgery. These potential complications can include bleeding, infection, damage to surrounding organs such as the bladder, bowel, or ureters, and adverse reactions to anesthesia. Another risk is the formation of scar tissue (adhesions). If both ovaries are removed in premenopausal women, it can lead to early menopause, resulting in symptoms like hot flashes, vaginal dryness, and bone density loss. This is a significant consideration for patients and their healthcare providers.
Oophorectomy Recovery: Timeline and Post-Surgery Care
The oophorectomy recovery time largely depends on the type of surgery performed (laparoscopic versus open) and the individual’s overall health. For laparoscopic oophorectomy, patients typically go home the same day or the next day and can resume light activities within a few days to a week. Full recovery, including returning to more strenuous activities, usually takes about two to four weeks. Open oophorectomy, being more invasive, generally requires a longer hospital stay (2-4 days) and a recovery period of four to six weeks, or sometimes longer, before full activity can be resumed.
Post-surgery care is crucial for a smooth recovery and to minimize complications. Key aspects include:
- Pain Management: Prescription or over-the-counter pain relievers will be recommended to manage discomfort at the incision sites.
- Wound Care: Keeping incision sites clean and dry is essential to prevent infection. Patients will receive specific instructions on how to care for their wounds.
- Activity Restrictions: Patients are typically advised to avoid heavy lifting, strenuous exercise, and sexual activity for several weeks to allow internal healing. Gradual increase in activity is encouraged.
- Monitoring for Complications: Patients should watch for signs of infection (fever, redness, swelling, pus at the incision site), excessive bleeding, severe pain, or difficulty urinating or having a bowel movement, and report them to their doctor immediately.
- Hormone Replacement Therapy (HRT): If both ovaries are removed in a premenopausal woman, HRT may be considered to manage menopausal symptoms and reduce long-term health risks associated with estrogen deficiency, such as osteoporosis and cardiovascular disease. This decision is made in consultation with a healthcare provider, weighing individual risks and benefits.