Throat Cancer Treatment Options
Understanding the various throat cancer treatment options is crucial for patients and their families. This article provides a comprehensive overview of current therapies, recovery expectations, and emerging innovations to help navigate this complex journey.
Key Takeaways
- Throat cancer treatment involves a multidisciplinary approach, often combining surgery, radiation, and systemic therapies.
- Treatment plans are highly personalized, depending on the cancer’s stage, location, and the patient’s overall health.
- Managing throat cancer treatment side effects is an integral part of care, focusing on improving quality of life during and after therapy.
- Recovery timelines vary significantly, and throat cancer treatment success rates are influenced by early detection and comprehensive care.
- Ongoing research is continually introducing new treatments for throat cancer, including personalized medicine and targeted therapies.
Primary Throat Cancer Treatment Options
When considering what are the treatment options for throat cancer, primary therapies often involve localized approaches designed to remove or destroy cancer cells directly at the tumor site. These are foundational types of throat cancer treatments and are frequently used in early-stage disease or as part of a multimodal strategy.
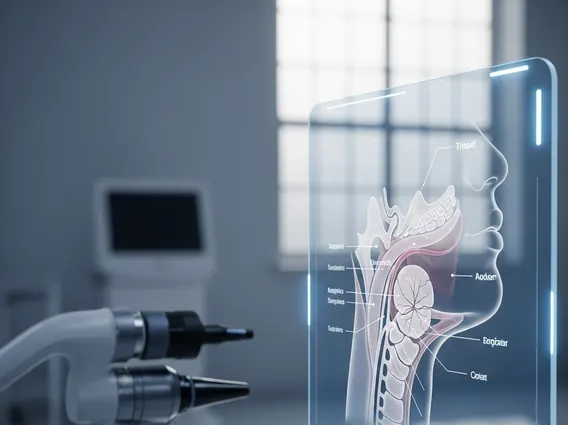
Surgical Interventions
Surgery is a common approach for many throat cancers, especially in earlier stages. The goal is to remove the tumor and a margin of healthy tissue around it. The specific surgical procedure depends on the tumor’s size, location, and extent.
- Laryngectomy: Removal of part or all of the voice box (larynx), often necessary for laryngeal cancers.
- Pharyngectomy: Removal of part of the pharynx (throat).
- Neck Dissection: Removal of lymph nodes in the neck if cancer has spread or is suspected to have spread.
- Transoral Robotic Surgery (TORS): A minimally invasive technique using robotic arms to access and remove tumors through the mouth, reducing the need for external incisions and potentially preserving more normal tissue.
Advances in surgical techniques aim to preserve speech and swallowing functions whenever possible, significantly impacting a patient’s quality of life post-treatment.
Radiation Therapy Approaches
Radiation therapy uses high-energy rays to kill cancer cells. It can be used as a primary treatment, particularly for early-stage throat cancers, or in combination with surgery or chemotherapy. It can also be used after surgery to destroy any remaining cancer cells or to alleviate symptoms in advanced cases.
- External Beam Radiation Therapy (EBRT): The most common type, where radiation is delivered from a machine outside the body.
- Intensity-Modulated Radiation Therapy (IMRT): A sophisticated form of EBRT that precisely shapes radiation beams to conform to the tumor’s shape, minimizing damage to surrounding healthy tissues and reducing throat cancer treatment side effects.
- Brachytherapy: Less common for throat cancer, this involves placing radioactive sources directly into or near the tumor.
A typical course of radiation therapy for throat cancer can last several weeks, with daily treatments five days a week.
Systemic and Targeted Therapies
Beyond localized treatments, systemic therapies work throughout the body, targeting cancer cells that may have spread beyond the primary tumor. These are often used for more advanced cancers or in conjunction with surgery and radiation.
Chemotherapy and Immunotherapy
Chemotherapy involves drugs that kill fast-growing cells, including cancer cells. It can be given intravenously or orally. For throat cancer, chemotherapy is often used in combination with radiation therapy (chemoradiation) to enhance its effectiveness, or as a primary treatment for advanced or metastatic disease. Common side effects include fatigue, nausea, hair loss, and increased risk of infection.
Immunotherapy represents a significant advancement in throat cancer treatment. These drugs work by boosting the body’s own immune system to recognize and destroy cancer cells. Checkpoint inhibitors, a type of immunotherapy, block proteins that prevent the immune system from attacking cancer. They are used for recurrent or metastatic throat cancers, particularly those that have not responded to other treatments. The side effect profile for immunotherapy differs from chemotherapy, often involving immune-related adverse events.
Targeted Drug Treatments
Targeted therapy drugs are designed to interfere with specific molecules involved in cancer growth and progression, with less harm to healthy cells compared to traditional chemotherapy. These treatments often require genetic testing of the tumor to identify specific mutations or biomarkers that the drugs can target. For throat cancer, targeted therapies may focus on pathways like the epidermal growth factor receptor (EGFR). These treatments offer a more personalized approach, and their development is a key area for new treatments for throat cancer.
Navigating Recovery and Treatment Outcomes
Recovery from throat cancer treatment is a multifaceted process that extends beyond the cessation of active therapy. It involves managing the physical and emotional aftermath and understanding the potential for long-term outcomes.
Managing Side Effects and Complications
Patients undergoing throat cancer treatment often experience a range of side effects, which can vary depending on the specific therapies received. Common throat cancer treatment side effects include:
- Difficulty Swallowing (Dysphagia): Can result from surgery, radiation, or chemoradiation, potentially requiring dietary modifications or feeding tubes.
- Voice Changes: Surgery on the larynx or radiation to the vocal cords can alter voice quality, pitch, or strength.
- Dry Mouth (Xerostomia): A common side effect of radiation therapy to the head and neck, impacting taste and increasing dental issues.
- Fatigue: A pervasive side effect across all treatment modalities.
- Skin Irritation: Redness, soreness, and peeling in the treated area from radiation.
- Pain: Managed with medication and other supportive therapies.
Supportive care, including nutritional counseling, speech therapy, physical therapy, and pain management, is crucial for mitigating these effects and improving quality of life during and after treatment.
Recovery Timeline and Success Rates
The throat cancer treatment recovery time is highly variable, depending on the stage of cancer, the specific treatments administered, and the individual’s overall health and resilience. While some immediate side effects may subside within weeks or months, others, such as voice changes or swallowing difficulties, can be long-lasting or permanent, requiring ongoing rehabilitation.
Throat cancer treatment success rates are generally improving due to advancements in diagnosis and therapy. According to the American Cancer Society (ACS), the overall 5-year survival rate for laryngeal cancer is approximately 61%, but this varies significantly based on the stage at diagnosis. For localized laryngeal cancer, the 5-year survival rate is around 78%, dropping to 47% if the cancer has spread regionally, and 33% if it has metastasized to distant parts of the body. Early detection and adherence to treatment plans are critical factors influencing these outcomes.
Emerging Innovations in Throat Cancer Treatment
The field of oncology is continuously evolving, bringing forth promising new treatments for throat cancer that aim for greater efficacy and fewer side effects.
Advancements in Personalized Medicine
Personalized medicine, also known as precision medicine, tailors treatment strategies to an individual’s unique genetic and molecular profile of their cancer. This involves comprehensive genomic profiling of the tumor to identify specific mutations, biomarkers, or genetic alterations that drive cancer growth. This information then guides the selection of targeted therapies or immunotherapies that are most likely to be effective for that particular patient, moving away from a one-size-fits-all approach. This precision can lead to higher response rates and reduced toxicity.
Clinical Trials and Future Directions
Clinical trials are research studies that test new medical approaches, including drugs, surgical procedures, radiation therapies, and combinations of treatments. They are essential for developing new treatments for throat cancer and improving existing ones. Patients participating in clinical trials may gain access to cutting-edge therapies not yet widely available. Current research focuses on enhancing immunotherapy responses, developing novel targeted agents, refining radiation techniques, and integrating artificial intelligence for better diagnostic and treatment planning.
Finding the Right Care: Hospitals and Specialists
Choosing the right medical team and facility is paramount for effective throat cancer treatment. A multidisciplinary team approach is often considered the gold standard, involving head and neck surgeons, radiation oncologists, medical oncologists, speech pathologists, dietitians, and supportive care specialists.
When seeking the best hospitals for throat cancer treatment, consider institutions with:
- Extensive experience in treating various head and neck cancers.
- Access to advanced diagnostic and treatment technologies (e.g., IMRT, TORS).
- A robust multidisciplinary team that collaborates on individualized treatment plans.
- Comprehensive supportive care services, including rehabilitation and survivorship programs.
- Participation in clinical trials, offering access to innovative therapies.
Seeking a second opinion from a specialized cancer center can also provide valuable insights and ensure all possible treatment avenues are explored.
Frequently Asked Questions About Throat Cancer Treatment
How long does throat cancer treatment typically last?
The duration of throat cancer treatment varies significantly based on the cancer stage, type, and specific therapies. Surgery might be a single event followed by recovery, while radiation therapy often spans 5-7 weeks. Chemotherapy cycles can extend over several months, sometimes concurrently with radiation. Immunotherapy or targeted therapies may continue for longer periods. The entire active treatment phase can range from a few weeks to many months, followed by an extended recovery and monitoring period.
What are the main factors influencing throat cancer treatment success?
Several factors influence throat cancer treatment success rates. Key among these are the stage of cancer at diagnosis (earlier stages generally have better prognoses), the specific location and type of cancer cells, the patient’s overall health and ability to tolerate treatment, and the expertise of the medical team. Adherence to the prescribed treatment plan and diligent follow-up care also play crucial roles in achieving positive outcomes and managing potential recurrence.
Are there different types of throat cancer treatments for early vs. advanced stages?
Yes, the types of throat cancer treatments are often tailored to the cancer stage. Early-stage throat cancers (Stage I and II) are frequently treated with a single modality, such as surgery or radiation therapy, aiming for a cure. For advanced stages (Stage III and IV), a multimodal approach is common, combining surgery, radiation, and systemic therapies like chemotherapy or immunotherapy. Treatment for advanced disease focuses on controlling the cancer, improving symptoms, and extending survival.