Pnet
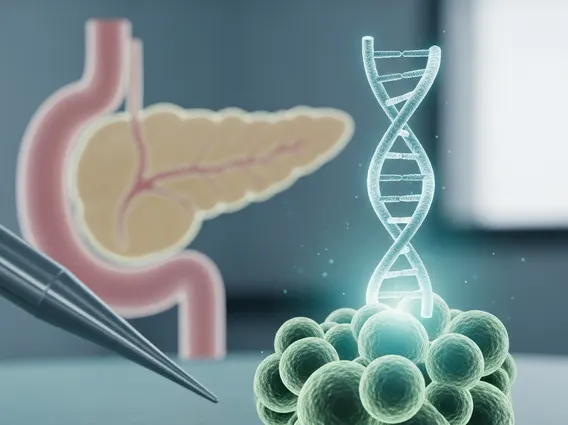
Pancreatic Neuroendocrine Tumor (PNET) is a rare form of cancer that originates in the neuroendocrine cells of the pancreas. These tumors differ significantly from the more common pancreatic adenocarcinoma, exhibiting a wide range of behaviors from slow-growing to aggressive.
Key Takeaways
- PNETs are rare cancers originating from specialized neuroendocrine cells in the pancreas, distinct from common pancreatic cancer.
- Their behavior varies, with some growing slowly and others more aggressively, and they can be functional (producing hormones) or non-functional.
- Diagnosis involves imaging, blood tests for hormones and tumor markers, and a definitive biopsy.
- Treatment is highly individualized, often including surgery, targeted therapies, chemotherapy, and somatostatin analogs.
- A multidisciplinary team approach is crucial for effective management and improved patient outcomes.
What is PNET (Pancreatic Neuroendocrine Tumor)?
PNET (Pancreatic Neuroendocrine Tumor) refers to a group of uncommon neoplasms that arise from the neuroendocrine cells scattered throughout the pancreas. These cells are responsible for producing hormones like insulin, glucagon, and somatostatin, which regulate various bodily functions. Unlike exocrine pancreatic cancers, which develop from the cells lining the pancreatic ducts, PNETs originate from these hormone-producing cells, giving them distinct characteristics and treatment approaches.
The Pnet meaning and definition highlight their rarity, accounting for less than 2% of all pancreatic cancers, according to the National Cancer Institute (NCI). This type of tumor can be either “functional,” meaning it produces an excess of hormones that cause specific symptoms (e.g., insulinoma producing insulin, gastrinoma producing gastrin), or “non-functional,” where it does not produce significant amounts of hormones and symptoms arise from the tumor’s size or spread. Understanding the nature of a PNET is crucial for effective management, as the prognosis and treatment strategies can vary widely depending on the tumor’s grade, stage, and whether it is functional or non-functional. This detailed information about Pnet helps distinguish it from other pancreatic conditions.
When considering Pnet explained, it’s important to note that these tumors can be benign or malignant, and their growth rate can range from indolent to highly aggressive. The classification and grading of PNETs are based on factors such as mitotic count and Ki-67 index, which help predict their biological behavior and guide therapeutic decisions.
Causes, Symptoms, and Diagnosis of PNET
The exact causes of PNETs are often unknown, but certain genetic syndromes are recognized risk factors. These include Multiple Endocrine Neoplasia type 1 (MEN1), Von Hippel-Lindau disease (VHL), neurofibromatosis type 1 (NF1), and tuberous sclerosis complex. Individuals with a family history of these conditions may have an increased predisposition to developing PNETs.
Symptoms of PNETs can be varied and often non-specific, making early diagnosis challenging. They largely depend on whether the tumor is functional or non-functional, and the specific hormone it produces. Common symptoms may include:
- Abdominal pain or discomfort
- Unexplained weight loss
- Jaundice (yellowing of skin and eyes) if the tumor blocks bile ducts
- Changes in bowel habits (diarrhea or constipation)
- Symptoms related to hormone overproduction (e.g., hypoglycemia from insulinoma, peptic ulcers from gastrinoma, skin rash and diabetes from glucagonoma).
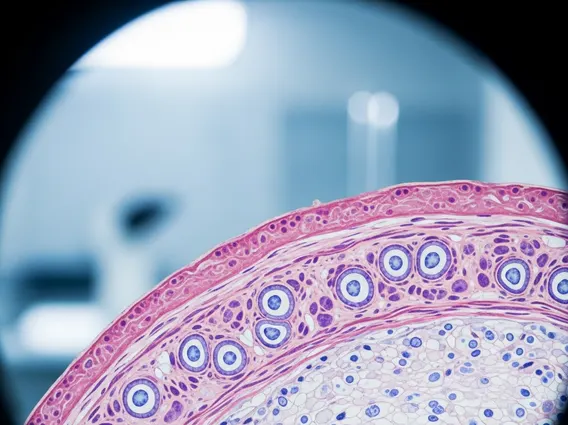
Diagnosing PNET typically involves a combination of imaging studies, blood tests, and biopsy. Imaging techniques such as computed tomography (CT) scans, magnetic resonance imaging (MRI), and somatostatin receptor scintigraphy (SRS, often using gallium-68 DOTATATE PET/CT) are used to locate the tumor and assess its spread. Blood tests can measure hormone levels (if a functional tumor is suspected) and tumor markers like chromogranin A. A definitive diagnosis is usually confirmed through a biopsy, where a small tissue sample is taken and examined under a microscope to determine the tumor type and grade.
Treatment and Management of PNET
Treatment for PNET is highly individualized, depending on the tumor’s size, location, grade, stage, and whether it is functional. A multidisciplinary team, including oncologists, surgeons, endocrinologists, and radiologists, typically collaborates to develop the most appropriate treatment plan.
Surgical resection is often the preferred treatment option for localized tumors that can be safely removed, offering the best chance for a cure. For tumors that are unresectable or have metastasized, various medical therapies are available:
- Somatostatin Analogs: Medications like octreotide and lanreotide can control hormone-related symptoms in functional tumors and may slow tumor growth in some cases.
- Targeted Therapies: Drugs such as everolimus and sunitinib target specific pathways involved in cancer cell growth and survival, proving effective for advanced PNETs.
- Chemotherapy: Certain chemotherapy regimens may be used, particularly for higher-grade or more aggressive tumors.
- Peptide Receptor Radionuclide Therapy (PRRT): This advanced therapy uses a radioactive substance attached to a somatostatin analog to deliver radiation directly to tumor cells that express somatostatin receptors.
- Liver-directed Therapies: For tumors that have spread to the liver, treatments like embolization or radiofrequency ablation may be used to control disease in this organ.
Ongoing surveillance and supportive care are integral to the long-term management of PNET patients. This includes regular monitoring for disease progression or recurrence, managing symptoms, and addressing treatment side effects to maintain quality of life. The choice of treatment strategy is continuously re-evaluated based on the patient’s response and disease evolution.