Penile Cancer Stages
Understanding the penile cancer stages is crucial for effective diagnosis, treatment planning, and determining prognosis. This article will explain how penile cancer is classified, the diagnostic methods used, and how staging impacts treatment and outlook.
Key Takeaways
- Penile cancer stages are determined using the TNM system, which assesses tumor size (T), lymph node involvement (N), and distant metastasis (M).
- Staging categorizes cancer from Stage 0 (carcinoma in situ) to Stage IV (advanced disease with distant spread).
- Accurate staging relies on a combination of physical exams, imaging tests, and definitive biopsy results.
- Treatment approaches are highly individualized, varying significantly based on the specific penile cancer stages.
- Prognosis generally improves with earlier detection and treatment, highlighting the importance of understanding penile cancer prognosis by stage.
Understanding Penile Cancer Stages
The classification of penile cancer stages provides a standardized way for medical professionals to describe the extent of the disease. This system helps guide treatment decisions and predict a patient’s outlook. Essentially, penile cancer staging explained involves evaluating how far the cancer has grown and whether it has spread to other parts of the body.
The TNM Staging System Explained
The most widely accepted system for staging penile cancer is the TNM system, developed by the American Joint Committee on Cancer (AJCC). This system considers three key factors:
- T (Tumor): Describes the size and extent of the primary tumor. This includes how deeply it has invaded the penile tissues, such as the glans, foreskin, shaft, or corpus cavernosum.
- N (Nodes): Indicates whether the cancer has spread to nearby lymph nodes, particularly those in the groin (inguinal lymph nodes). The number of affected nodes and the extent of their involvement are critical.
- M (Metastasis): Determines if the cancer has spread to distant parts of the body, such as the lungs, liver, or bones. This is known as distant metastasis.
Each of these factors is assigned a number or letter (e.g., T1, T2, N0, N1, M0, M1) to provide a precise description of the cancer’s extent. These individual classifications are then combined to determine the overall stage.
General Stage Categories (0-IV)
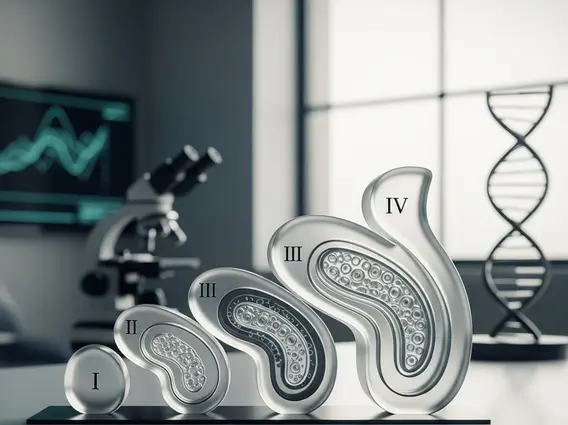
Based on the TNM classifications, penile cancer is grouped into general stages, ranging from 0 to IV:
- Stage 0 (Carcinoma in Situ): This is the earliest stage, where abnormal cells are found only in the top layer of the skin of the penis and have not invaded deeper tissues.
- Stage I: The cancer has grown into the connective tissue just beneath the skin but has not spread to blood vessels, lymphatic vessels, or lymph nodes.
- Stage II: The cancer has invaded deeper into the connective tissue, or into the corpus spongiosum or corpus cavernosum, but still without lymph node involvement or distant spread.
- Stage III: The cancer has spread to nearby lymph nodes in the groin, but not to distant sites. This stage is further divided based on the number and characteristics of the affected lymph nodes.
- Stage IV: This represents the most advanced penile cancer stages, where the cancer has either spread to distant organs (M1) or has extensively invaded regional lymph nodes and/or adjacent structures like the pubic bone or scrotum.
How Penile Cancer is Staged
Accurately determining how is penile cancer staged involves a comprehensive evaluation by a medical team. This process combines physical examinations with various diagnostic tests to assess the tumor’s characteristics and potential spread.
Diagnostic Tests and Procedures
Several diagnostic tools are employed to gather information for staging:
- Physical Examination: A thorough examination of the penis and groin area is the first step. The doctor will look for visible lesions, feel for lumps, and check for enlarged lymph nodes in the groin.
- Imaging Tests: These tests help visualize the extent of the tumor and check for spread.
- MRI (Magnetic Resonance Imaging): Often used to assess the depth of invasion within the penis.
- CT (Computed Tomography) Scan: Can be used to check for spread to lymph nodes in the pelvis and abdomen, as well as distant organs.
- PET (Positron Emission Tomography) Scan: Sometimes used to detect cancer cells that have spread throughout the body, especially in advanced cases.
- Ultrasound: May be used to examine the penis or groin lymph nodes.
- Sentinel Lymph Node Biopsy: For certain stages, this procedure identifies the first lymph node(s) to which cancer cells are most likely to spread. If these “sentinel” nodes are clear of cancer, it suggests the cancer has not spread to the lymph nodes.
Biopsy and Pathology Reports
The definitive step in staging is a biopsy. A small tissue sample from the suspicious area on the penis is removed and examined under a microscope by a pathologist. The pathology reports provide crucial information, including:
- Cancer Type: Most penile cancers are squamous cell carcinomas.
- Grade: Describes how abnormal the cancer cells look and how quickly they are likely to grow and spread (e.g., low-grade, high-grade).
- Depth of Invasion: Precisely measures how deeply the tumor has penetrated the penile tissues.
- Lymphovascular Invasion: Notes whether cancer cells are found in small blood vessels or lymphatic vessels, indicating a higher risk of spread.
The information from the biopsy, combined with imaging results and physical examination, allows the medical team to accurately determine the penile cancer stages.
Symptoms and Signs by Stage
Recognizing the stages of penile cancer symptoms is vital for early detection and improved outcomes. Symptoms can vary depending on how advanced the cancer is, from subtle changes in early stages to more pronounced signs in advanced disease.
Early Stage Indicators
In the early penile cancer stages, symptoms are often localized to the penis and may be mistaken for other, less serious conditions. Common early signs include:
- Skin Changes: A persistent sore, lump, or ulcer on the penis that does not heal. This might appear on the glans (head of the penis), foreskin, or shaft.
- Discoloration: Reddish-brown spots or patches on the skin of the penis.
- Rash or Growth: A persistent rash or wart-like growth that does not resolve with standard treatments.
- Discharge: Unusual or foul-smelling discharge from under the foreskin.
- Bleeding: Bleeding from the penis, especially from a lesion or under the foreskin.
- Thickening of the skin: A noticeable thickening or hardening of the skin on the penis.
These early indicators, while potentially subtle, warrant immediate medical evaluation to ensure timely diagnosis.
Advanced Stage Manifestations
As the cancer progresses to more advanced penile cancer stages, symptoms may become more severe and indicate spread beyond the penis:
- Groin Swelling: Enlarged lymph nodes in the groin area, which may feel like firm lumps. This is a significant sign of regional spread.
- Pain: Persistent pain in the penis, groin, or pelvic area.
- Urinary Issues: Difficulty urinating, changes in urine stream, or blood in the urine (hematuria) if the tumor affects the urethra.
- Weight Loss and Fatigue: Unexplained weight loss, loss of appetite, and persistent fatigue are general signs of advanced cancer.
- Bone Pain: If the cancer has metastasized to the bones, it can cause localized pain.
- Bowel Changes: In very advanced cases, if the cancer spreads to adjacent structures, it might affect bowel function.
Any of these advanced symptoms require urgent medical attention to manage the disease and improve quality of life.
Treatment Options for Penile Cancer Stages
Treatment for penile cancer is highly individualized, with choices largely dictated by the specific penile cancer stages at diagnosis. The goal is to remove the cancer while preserving as much penile function and appearance as possible.
Stage-Specific Therapies
Treatment strategies vary significantly:
- Early Stage Penile Cancer Treatment (Stages 0 and I):
- Topical Therapies: Creams like 5-fluorouracil (5-FU) or imiquimod may be used for very superficial cancers (Stage 0).
- Laser Ablation: Uses a focused beam of light to destroy cancer cells.
- Circumcision: If the cancer is confined to the foreskin.
- Wide Local Excision: Surgical removal of the tumor along with a margin of healthy tissue.
- Mohs Micrographic Surgery: A specialized technique that removes thin layers of skin containing cancer cells, examining each layer until no cancer remains, minimizing tissue removal.
- Advanced Penile Cancer Stages (Stages II, III, and IV):
- Surgery: More extensive surgical procedures may be necessary, such as partial penectomy (removal of part of the penis) or total penectomy (removal of the entire penis) for larger or deeply invasive tumors. Lymph node dissection (removal of groin lymph nodes) is often performed to check for and remove cancerous nodes.
- Radiation Therapy: Can be used alone or in combination with surgery or chemotherapy, especially for tumors that are not surgically removable or to target lymph nodes.
- Chemotherapy: May be used before surgery (neoadjuvant) to shrink large tumors, after surgery (adjuvant) to kill remaining cancer cells, or for metastatic disease (Stage IV) to control symptoms and slow progression.
- Targeted Therapy and Immunotherapy: Newer treatments that specifically target cancer cells or boost the body’s immune response are being investigated and may be used in certain advanced cases.
Multidisciplinary Care Approaches
Effective management of penile cancer typically involves a multidisciplinary team of specialists. This team may include urologists, surgical oncologists, radiation oncologists, medical oncologists, pathologists, and reconstructive surgeons. This collaborative approach ensures that all aspects of the patient’s condition are considered, leading to a tailored treatment plan that optimizes outcomes and supports the patient through their journey.
Penile Cancer Prognosis by Stage
Understanding the penile cancer prognosis by stage is a critical aspect of diagnosis and treatment planning. The outlook for patients with penile cancer is highly dependent on how early the cancer is detected and treated, as well as other individual factors.
Survival Rates and Outlook
Generally, the earlier the stage of penile cancer, the better the prognosis. Survival rates are often discussed in terms of the 5-year relative survival rate, which compares the survival of people with penile cancer to the survival of people in the general population.
While specific percentages can vary based on the source and population studied, the trend is consistent:
| Penile Cancer Stage | General Prognosis | 5-Year Relative Survival Rate (Approximate) |
|---|---|---|
| Stage 0 (Carcinoma in Situ) | Excellent, nearly 100% cure rate with appropriate treatment. | ~100% |
| Stage I | Very good, high chance of cure with local treatment. | ~85-90% |
| Stage II | Good, but risk of recurrence or spread is higher than Stage I. | ~60-70% |
| Stage III | Fair, as cancer has spread to regional lymph nodes. Aggressive treatment is needed. | ~30-50% |
| Stage IV | Poor, as cancer has spread to distant organs or extensively to regional nodes. Focus shifts to managing symptoms and extending life. | ~10-20% |
It’s important to note that these figures are averages and do not predict an individual’s specific outcome. Advances in treatment continually improve these statistics. According to the American Cancer Society, early detection significantly improves these outcomes.
Factors Influencing Prognosis
Beyond the penile cancer stages, several other factors can influence an individual’s prognosis:
- Tumor Grade: Higher-grade tumors (more aggressive-looking cells) tend to have a worse prognosis than lower-grade tumors.
- Lymph Node Involvement: The number of affected lymph nodes, whether they are fixed or mobile, and whether the cancer has spread outside the lymph node capsule significantly impact prognosis.
- Patient’s Overall Health: General health, presence of other medical conditions, and ability to tolerate treatment can affect outcomes.
- Response to Treatment: How well the cancer responds to initial therapy is a key indicator.
- Surgical Margins: Achieving clear surgical margins (no cancer cells at the edge of the removed tissue) is crucial for preventing local recurrence.
- Presence of Lymphovascular Invasion: If cancer cells are found in small blood or lymphatic vessels, it indicates a higher risk of spread and a potentially worse prognosis.
Patients should discuss their specific prognosis with their healthcare team, who can provide the most accurate information based on their individual case.
Frequently Asked Questions
What are the stages of penile cancer?
Penile cancer is typically staged using a system from Stage 0 to Stage IV. Stage 0, or carcinoma in situ, indicates cancer cells are only on the surface. Stage I means the cancer has invaded slightly deeper but is localized. Stage II involves deeper invasion into the penis without lymph node spread. Stage III signifies spread to regional lymph nodes in the groin. Stage IV is the most advanced, indicating extensive regional spread or distant metastasis to other organs. These stages guide treatment and prognosis.
How is penile cancer staged?
Penile cancer is staged through a comprehensive process involving physical examination, imaging tests, and a definitive biopsy. Doctors assess the tumor’s size and depth (T), check for lymph node involvement (N) using physical exams, imaging (CT, MRI), and sometimes sentinel lymph node biopsy, and look for distant spread (M) with imaging. The pathology report from the biopsy provides crucial details about the cancer type, grade, and invasion depth, all of which are combined to assign an accurate stage.
What is the prognosis for early stage penile cancer?
The prognosis for early stage penile cancer (Stages 0 and I) is generally very good, with high rates of successful treatment and long-term survival. For carcinoma in situ (Stage 0), the cure rate approaches 100% with appropriate local therapies. For Stage I, the 5-year relative survival rate is typically around 85-90%. Early detection and prompt treatment are key factors in achieving these excellent outcomes, emphasizing the importance of recognizing initial symptoms and seeking medical advice.