Osteosarcoma Treatment Options
Osteosarcoma is the most common type of primary bone cancer, predominantly affecting children, adolescents, and young adults. Understanding the various osteosarcoma treatment options is crucial for patients and their families navigating this challenging diagnosis.
Key Takeaways
- Osteosarcoma treatment is highly individualized, based on factors like tumor characteristics and patient health.
- A multidisciplinary team approach, involving various specialists, is fundamental for comprehensive care.
- Primary treatment modalities include surgical removal of the tumor and chemotherapy, often used before and after surgery.
- Emerging therapies, such as targeted drugs and immunotherapy, are expanding the landscape of new osteosarcoma treatments.
- Long-term follow-up and management of potential side effects are integral components of post-treatment care.
Understanding Osteosarcoma Treatment Approaches
Effective osteosarcoma treatment requires a comprehensive and strategic approach, beginning from the moment of diagnosis. The complexity of this bone cancer necessitates a well-coordinated plan tailored to each individual.
Initial Diagnosis and Staging
The journey of understanding osteosarcoma treatment begins with an accurate diagnosis and meticulous staging. This process typically involves a combination of imaging studies, such as X-rays, MRI, CT scans, and PET scans, alongside a biopsy of the tumor. The biopsy is critical for confirming the diagnosis and determining the specific characteristics of the cancer cells. Staging, which assesses the tumor’s size, location, and whether it has spread (metastasized), is paramount in guiding the initial osteosarcoma treatment guidelines. For instance, approximately 15-20% of patients present with detectable metastatic disease at diagnosis, most commonly in the lungs, according to the American Cancer Society.
Multidisciplinary Care Teams
A cornerstone of modern osteosarcoma treatment options is the multidisciplinary care team. This collaborative group typically includes pediatric or medical oncologists, orthopedic surgeons specializing in oncology, radiation oncologists, radiologists, pathologists, rehabilitation specialists, and psychosocial support staff. Their combined expertise ensures that every aspect of the patient’s condition is considered, leading to a holistic and integrated treatment strategy. This team approach is vital for developing the most effective plan, from initial diagnosis through long-term follow-up, optimizing outcomes and quality of life.
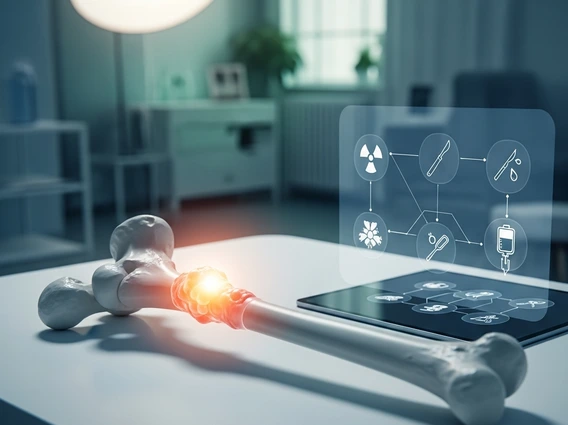
Primary Osteosarcoma Treatment Modalities
The core of what are osteosarcoma treatments primarily revolves around two key modalities: surgical removal of the tumor and chemotherapy. These are often used in combination to achieve the best possible outcomes.
Surgical Resection Techniques
Surgery is a critical component of osteosarcoma treatment, aiming to remove the entire tumor with clear margins (a rim of healthy tissue around the tumor). The type of surgery depends heavily on the tumor’s location and size. Limb-sparing surgery, which involves removing the cancerous bone and replacing it with a metal prosthesis, bone graft, or a combination, is often preferred to preserve limb function. This approach is successful in approximately 85-90% of cases, avoiding amputation, as reported by the National Cancer Institute. In situations where the tumor is extensive or involves critical structures, amputation may be necessary to ensure complete removal of the cancer. Post-surgical rehabilitation is essential for regaining strength and mobility.
Chemotherapy Protocols
Chemotherapy plays a vital role in osteosarcoma treatment, often administered both before (neoadjuvant) and after (adjuvant) surgery. Neoadjuvant chemotherapy helps shrink the tumor, making it easier to remove surgically, and also targets any microscopic cancer cells that may have spread but are not yet detectable. Adjuvant chemotherapy aims to kill any remaining cancer cells after surgery, reducing the risk of recurrence. Common chemotherapy drugs used include methotrexate, doxorubicin, cisplatin, and ifosfamide. The specific protocol, dosage, and duration are determined by factors such as the tumor’s response, patient tolerance, and overall health. This systematic approach significantly improves survival rates, with 5-year survival rates for localized osteosarcoma now exceeding 70% in many centers, a substantial improvement from historical figures before chemotherapy integration.
New and Emerging Therapies for Osteosarcoma
The landscape of osteosarcoma treatment is continuously evolving, with ongoing research leading to the development of innovative therapies. These new osteosarcoma treatments offer hope for patients, especially those with recurrent or metastatic disease.
Targeted Therapies and Immunotherapy
Targeted therapies are a class of drugs designed to specifically attack cancer cells by interfering with particular molecules involved in tumor growth and progression, while minimizing harm to healthy cells. For osteosarcoma, research is exploring agents that target pathways like mTOR, VEGF, and receptor tyrosine kinases. Immunotherapy, another promising avenue, works by harnessing the body’s own immune system to recognize and destroy cancer cells. This involves using drugs like checkpoint inhibitors, which release the brakes on immune cells, allowing them to mount a stronger attack against the tumor. While still largely under investigation for osteosarcoma, these types of osteosarcoma therapy represent a significant shift from traditional chemotherapy, offering more precise and potentially less toxic options.
Clinical Trials and Research
Participation in clinical trials is a crucial way for patients to access new osteosarcoma treatments that are not yet widely available. These research studies test the safety and effectiveness of new drugs, combinations of existing therapies, or novel surgical and radiation techniques. Clinical trials are rigorously regulated and play an indispensable role in advancing medical knowledge and improving outcomes for future patients. For individuals facing osteosarcoma, discussing the possibility of enrolling in a clinical trial with their medical team can provide access to cutting-edge therapies and contribute to the collective effort to find the best treatment for osteosarcoma.
Personalizing Your Osteosarcoma Treatment Plan
Given the aggressive nature and varied presentations of osteosarcoma, developing a personalized osteosarcoma treatment plan is essential. This ensures that the chosen approach is optimally suited to the individual patient’s unique circumstances.
Factors Influencing Treatment Choices
Several factors influence the selection of the best treatment for osteosarcoma. These include the tumor’s location, size, and grade (how aggressive it appears under a microscope), as well as whether the cancer has spread. Patient-specific factors such as age, overall health, and response to initial chemotherapy also play a significant role. For instance, a younger patient with a localized tumor might be a candidate for more intensive chemotherapy regimens and limb-sparing surgery, while an older patient with comorbidities might require a modified approach. The goal is always to maximize the chance of cure while minimizing side effects and preserving quality of life.
Shared Decision-Making
Understanding osteosarcoma treatment involves active participation from the patient and their family in the decision-making process. Shared decision-making means that the medical team provides comprehensive information about all available types of osteosarcoma therapy, including their potential benefits, risks, and side effects. Patients and their families then have the opportunity to ask questions, express their values and preferences, and ultimately collaborate with their doctors to choose the treatment plan that aligns best with their goals and lifestyle. This collaborative approach empowers patients and ensures that their voice is heard throughout their treatment journey.
Life After Osteosarcoma Treatment
Completing active osteosarcoma treatment is a significant milestone, but the journey continues with ongoing surveillance and management of potential long-term effects. This phase is crucial for ensuring sustained health and well-being.
Follow-up and Surveillance
After completing primary therapy, patients enter a critical phase of follow-up and surveillance. This typically involves regular physical examinations, imaging studies (such as chest X-rays or CT scans to monitor for lung metastases, and MRI scans of the primary site), and blood tests. The frequency of these appointments gradually decreases over time but can extend for many years. The primary goal of this surveillance is to detect any signs of cancer recurrence early, when it is most treatable, and to monitor for any late effects of the treatment. Adherence to these osteosarcoma treatment guidelines for follow-up is vital for long-term success.
Managing Long-Term Effects
While osteosarcoma treatment is life-saving, it can sometimes lead to long-term side effects. These may include issues related to bone health (e.g., fractures, growth discrepancies), organ function (e.g., heart or kidney problems from chemotherapy), nerve damage, or psychological impacts such as anxiety or depression. Rehabilitation services, including physical and occupational therapy, are often necessary to address functional limitations resulting from surgery or other treatments. A comprehensive survivorship care plan, developed with the medical team, helps patients manage these potential issues, ensuring they receive appropriate support and interventions to maintain the best possible quality of life.
Frequently Asked Questions
What is the primary goal of osteosarcoma treatment?
The primary goal of osteosarcoma treatment is to cure the cancer and prevent its recurrence, while also preserving limb function and maintaining the patient’s quality of life. This involves a strategic combination of therapies, typically surgery to remove the tumor and chemotherapy to eliminate cancer cells throughout the body. The ultimate aim is to achieve a disease-free state and enable patients to return to a full and active life, with ongoing monitoring to ensure long-term well-being.
How important is a multidisciplinary team in osteosarcoma care?
A multidisciplinary team is critically important in osteosarcoma care because it brings together diverse medical specialists to create a comprehensive and individualized treatment plan. This collaborative approach ensures that all aspects of the disease—from diagnosis and surgical planning to chemotherapy, rehabilitation, and psychosocial support—are expertly addressed. Such coordinated care optimizes treatment outcomes, minimizes complications, and provides holistic support for patients and their families throughout the challenging journey of osteosarcoma treatment.
Are there specific dietary recommendations during osteosarcoma treatment?
While there are no specific dietary recommendations that can cure osteosarcoma, maintaining good nutrition is crucial during osteosarcoma treatment. A balanced diet rich in protein, vitamins, and minerals helps support the immune system, promotes healing, and helps patients tolerate treatments better. It’s important to consult with a registered dietitian or healthcare provider for personalized dietary advice, especially if experiencing side effects like nausea or appetite loss. Avoid unverified “cancer diets” and always prioritize evidence-based nutritional guidance from your medical team.
