Diagnosis, Screening, and Early Detection of Esophageal Cancer
Esophageal cancer is a serious condition that, when caught early, offers significantly better treatment outcomes. Understanding the subtle symptoms, knowing when screening is appropriate, and recognizing the comprehensive diagnostic process are crucial steps in combating this disease.
Key Takeaways
- Early symptoms of esophageal cancer are often subtle and can be easily mistaken for less serious conditions, making vigilance important.
- Esophageal cancer screening guidelines primarily target individuals at high risk, such as those with Barrett’s esophagus or a strong history of chronic reflux.
- The definitive esophageal cancer diagnosis involves a combination of imaging tests, endoscopy, and biopsy.
- Importance of early esophageal cancer diagnosis cannot be overstated, as it significantly improves prognosis and treatment effectiveness.
- If you experience persistent symptoms like difficulty swallowing or unexplained weight loss, seek medical evaluation promptly.
Symptoms and Early Warning Signs
Recognizing the symptoms of early esophageal cancer can be challenging because they are often subtle and non-specific, frequently mimicking common digestive issues. In its initial stages, the disease may present with no noticeable symptoms at all, which underscores the difficulty in esophageal cancer early detection methods without targeted screening for high-risk individuals. However, as the tumor grows, certain signs tend to emerge, prompting individuals to seek medical attention.
One of the most common and significant indicators is dysphagia, or difficulty swallowing. Initially, this might be experienced as a sensation of food getting stuck, particularly with solid foods, and it tends to worsen over time, eventually affecting liquids. Other important indicators that answer the question, “What are the signs of esophageal cancer?” include unexplained weight loss, persistent heartburn or indigestion that doesn’t respond to medication, and chest pain or pressure, which can sometimes be confused with heart problems. It’s vital to note that while these symptoms can be indicative of esophageal cancer, they are also common in many benign conditions, necessitating a thorough medical evaluation.
Beyond dysphagia and weight loss, patients might also experience chronic coughing, hoarseness, or even regurgitation of food. The presence of these symptoms, especially when persistent or worsening, should trigger a consultation with a healthcare professional. According to the American Cancer Society, only about 20% of esophageal cancers are found at an early stage, highlighting the critical need for awareness and prompt investigation of persistent symptoms, particularly in individuals with known risk factors.
- Difficulty Swallowing (Dysphagia): Often starts with solids, progressing to liquids.
- Unexplained Weight Loss: Significant weight loss without changes in diet or exercise.
- Persistent Heartburn or Indigestion: Not relieved by over-the-counter medications.
- Chest Pain or Pressure: Discomfort or burning sensation behind the breastbone.
- Chronic Cough or Hoarseness: Persistent cough or voice changes not related to a cold.
- Regurgitation: Bringing up undigested food.
Esophageal Cancer Screening Options
Unlike some other cancers, there are no universal esophageal cancer screening guidelines for the general population. Screening is typically reserved for individuals identified as being at a significantly higher risk due to specific pre-existing conditions or lifestyle factors. The primary goal of screening in these high-risk groups is to detect precancerous changes, such as Barrett’s esophagus, before they progress to invasive cancer, thereby improving the chances of successful treatment.
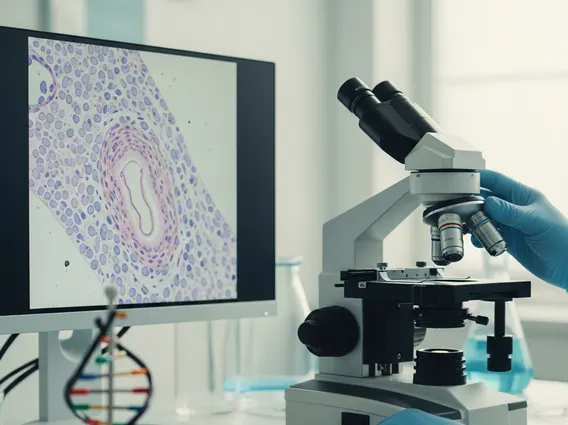
The most common and effective of the esophageal cancer screening options is endoscopy with biopsy. During this procedure, a thin, flexible tube with a camera (endoscope) is passed down the throat into the esophagus, allowing the doctor to visually inspect the lining. If abnormal areas are found, small tissue samples (biopsies) are taken and examined under a microscope for signs of dysplasia or cancer. This surveillance is particularly important for individuals diagnosed with Barrett’s esophagus, a condition where the normal lining of the esophagus is replaced by tissue similar to that lining the intestine, often due to chronic acid reflux. The American College of Gastroenterology recommends endoscopic surveillance for patients with Barrett’s esophagus, with frequency depending on the degree of dysplasia.
Other potential screening methods, though less common or still under investigation for widespread use, include specialized imaging techniques or molecular markers. However, for now, regular endoscopic surveillance remains the cornerstone for high-risk individuals. It is crucial for those with long-standing gastroesophageal reflux disease (GERD), a history of smoking, heavy alcohol consumption, or a family history of esophageal cancer to discuss their risk factors with a doctor to determine if screening is appropriate for them.
The Esophageal Cancer Diagnosis Process
When symptoms suggest the possibility of esophageal cancer, a comprehensive diagnostic process is initiated to confirm the presence of the disease and determine its stage. This process, which directly addresses “How is esophageal cancer diagnosed?“, involves several steps, starting with a detailed medical history and physical examination. The ultimate goal is to achieve an accurate esophageal cancer diagnosis, which is critical for planning effective treatment.
Initial investigations often include imaging studies. A barium swallow, also known as an esophagram, involves drinking a liquid containing barium, which coats the lining of the esophagus and makes it visible on X-rays. This can reveal abnormalities such as narrowing, blockages, or irregular areas. Further imaging may include computed tomography (CT) scans of the chest and abdomen, and sometimes a positron emission tomography (PET) scan, to assess the extent of the disease and check for spread to other organs. These scans are vital for staging the cancer.
Initial Diagnostic Steps
The first step in diagnosing esophageal cancer typically involves a thorough evaluation of the patient’s symptoms and medical history. If symptoms like persistent dysphagia or unexplained weight loss are present, the doctor will likely recommend an upper endoscopy. This procedure is central to the diagnostic process. During an endoscopy, a gastroenterologist inserts a thin, flexible tube equipped with a light and camera down the throat to visualize the esophagus directly. Any suspicious areas, such as masses, ulcers, or changes in the mucosal lining, can be identified. If abnormalities are seen, small tissue samples (biopsies) are taken for pathological examination.
The biopsy is the definitive test for confirming cancer. A pathologist examines the tissue under a microscope to determine if cancer cells are present and, if so, the specific type of esophageal cancer (e.g., adenocarcinoma or squamous cell carcinoma). This initial step is crucial for establishing a diagnosis and guiding subsequent staging and treatment decisions. Without a biopsy, a definitive diagnosis cannot be made, even if imaging suggests a tumor.
Confirmatory and Staging Procedures
Once cancer is confirmed by biopsy, further tests are necessary to determine the stage of the cancer, which refers to its size, location, and whether it has spread. This staging process is vital for determining the most appropriate treatment plan. Endoscopic ultrasound (EUS) is often used, combining endoscopy with ultrasound imaging to provide detailed pictures of the esophageal wall and nearby lymph nodes, helping to assess the depth of tumor invasion and regional lymph node involvement. This offers a more precise local staging than CT scans alone.
Additional imaging tests, such as a CT scan of the chest, abdomen, and pelvis, are performed to look for distant spread (metastasis) to other organs. A PET scan may also be used to detect cancer cells throughout the body, as these cells tend to absorb more of the radioactive tracer used in the scan. In some cases, a laparoscopy (a minimally invasive surgical procedure) may be performed to directly examine the abdominal cavity for signs of spread. All these procedures collectively paint a complete picture of the cancer’s extent, informing the multidisciplinary team on the best course of action.
Why Early Detection Matters
The importance of early esophageal cancer diagnosis cannot be overstated, as it directly correlates with significantly improved prognosis and treatment outcomes. Esophageal cancer, when detected at an advanced stage, often has a poor prognosis because it may have spread to distant organs, making curative treatment much more challenging. However, when identified in its earliest stages, particularly when it is confined to the superficial layers of the esophagus or is still a precancerous condition like high-grade dysplasia, the chances of successful treatment and long-term survival increase dramatically.
Esophageal cancer early detection methods allow for less invasive and more effective treatment options. For instance, very early-stage cancers or high-grade dysplasia can sometimes be treated with endoscopic procedures, such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD), which remove the cancerous or precancerous tissue without requiring major surgery. In contrast, advanced cancers often necessitate extensive surgery, chemotherapy, radiation therapy, or a combination of these, which carry greater risks and side effects, and may only aim for palliation rather than cure.
According to data from the National Cancer Institute’s SEER program, the 5-year relative survival rate for localized esophageal cancer (cancer that has not spread beyond the esophagus) is approximately 47%. This figure drops significantly to about 25% if the cancer has spread to regional lymph nodes and further declines to around 5% if it has metastasized to distant parts of the body. These statistics powerfully illustrate why vigilance for symptoms and adherence to recommended screening for high-risk individuals are paramount. Early intervention not only saves lives but also preserves quality of life by enabling less aggressive treatments.
Frequently Asked Questions
What are the primary risk factors for esophageal cancer?
The main risk factors for esophageal cancer include chronic gastroesophageal reflux disease (GERD), which can lead to Barrett’s esophagus, a precancerous condition. Other significant factors are smoking, heavy alcohol consumption, obesity, and a diet low in fruits and vegetables. Certain genetic syndromes and a history of radiation therapy to the chest can also increase risk. Understanding these factors is crucial for individuals to assess their personal risk and discuss potential screening options with their healthcare provider.
Can lifestyle changes reduce the risk of esophageal cancer?
Yes, adopting certain lifestyle changes can significantly reduce the risk of developing esophageal cancer. Quitting smoking and reducing alcohol intake are among the most impactful steps. Maintaining a healthy weight through diet and exercise can help manage GERD and reduce obesity-related risks. Eating a balanced diet rich in fruits, vegetables, and whole grains also contributes to overall health and may lower cancer risk. Managing chronic GERD effectively with medication or lifestyle adjustments is also vital.
How often should individuals with Barrett’s esophagus be screened?
The frequency of screening for individuals with Barrett’s esophagus depends on the presence and grade of dysplasia. For those with no dysplasia, surveillance endoscopy is typically recommended every 3-5 years. If low-grade dysplasia is found, screening may be advised every 6-12 months, or treatment options to eradicate the dysplasia might be considered. For high-grade dysplasia, more frequent surveillance (every 3 months) or immediate intervention, such as endoscopic ablation or resection, is usually recommended due to the higher risk of progression to cancer. Your doctor will tailor the screening schedule based on your specific condition.