Key Takeaways
- Tongue cancer is primarily squamous cell carcinoma, affecting either the oral tongue or the base of the tongue.
- Early detection is vital, with key early signs of tongue cancer including persistent sores, lumps, or red/white patches on the tongue.
- Major causes of tongue cancer include tobacco and alcohol use, as well as HPV infection.
- Diagnosis involves a physical exam and biopsy, followed by imaging to determine the stage.
- Tongue cancer treatment options typically involve surgery, radiation, and/or chemotherapy, with tongue cancer prognosis depending heavily on the stage at diagnosis.
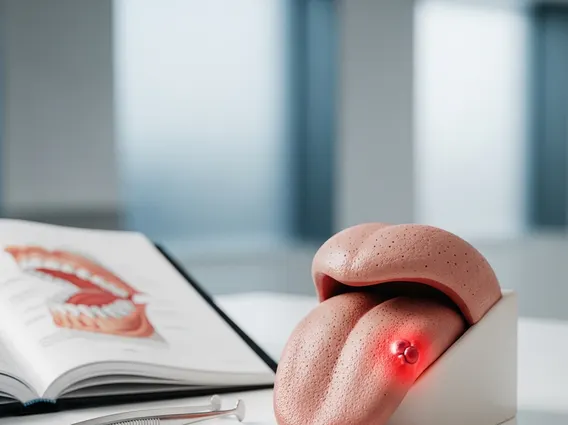
What is Tongue Cancer?
Tongue cancer refers to the uncontrolled growth of abnormal cells that form a tumor on the tongue. It is a significant subset of oral cavity cancers, which are part of the broader category of head and neck cancers. This malignancy can develop on the front two-thirds of the tongue, known as the oral tongue, or at the back, which is the base of the tongue. The distinction is important because cancers of the oral tongue are often more visible and detectable earlier, while base of tongue cancers can be harder to spot and are frequently associated with human papillomavirus (HPV) infection.
Types of Oral Cancer Affecting the Tongue
The vast majority of tongue cancer cases, approximately 90%, are classified as squamous cell carcinomas. These cancers originate in the thin, flat squamous cells that line the surface of the tongue. Less common types of cancer that can affect the tongue include minor salivary gland cancers, lymphomas, and sarcomas, but these are rare compared to squamous cell carcinoma.
Prevalence and Demographics
Oral cancers, including those affecting the tongue, represent a notable public health concern globally. According to the World Health Organization (WHO), cancers of the lip and oral cavity are among the top 20 most common cancers worldwide. In the United States, the National Cancer Institute (NCI) estimates that oral and pharyngeal cancers affect tens of thousands of individuals annually, with a significant portion involving the tongue. While historically more common in older men, the incidence of HPV-related base of tongue cancers is rising in younger populations, affecting both men and women. Factors such as geographical location, socioeconomic status, and access to healthcare can also influence prevalence rates.
Recognizing Early Signs and Symptoms
Early detection is paramount for improving the tongue cancer prognosis. Being aware of the early signs of tongue cancer can lead to prompt medical evaluation and timely intervention. Many of these signs can mimic less serious conditions, making professional medical assessment crucial for an accurate diagnosis.
Visible Changes and Sores
One of the most common symptoms of tongue cancer is a persistent sore or ulcer on the tongue that does not heal within two weeks. This lesion may appear as a white or red patch, often referred to as leukoplakia (white patch) or erythroplakia (red patch). Erythroplakia, in particular, has a higher potential for malignancy. Other visible changes include a persistent lump or thickening on the tongue, or a feeling of numbness in part of the tongue or mouth. Any unexplained bleeding from the tongue or mouth should also be investigated.
Pain and Functional Difficulties
Beyond visible changes, tongue cancer can manifest through various functional difficulties and pain. Patients may experience persistent pain in the tongue, mouth, or throat that does not subside. This pain can sometimes radiate to the ear. Difficulty or pain when swallowing (dysphagia), chewing, or moving the tongue or jaw are also significant warning signs. Changes in speech, such as slurring or difficulty articulating words, can occur as the tumor grows and affects tongue mobility. Unexplained weight loss may also be a symptom in more advanced stages.
Causes and Risk Factors for Tongue Cancer
Understanding the causes of tongue cancer is essential for prevention and risk reduction. While not every individual exposed to risk factors will develop the disease, these factors significantly increase the likelihood.
Lifestyle and Environmental Factors
The most prominent risk factors for tongue cancer are related to lifestyle choices. Tobacco use, including smoking cigarettes, cigars, pipes, and using smokeless tobacco products, is a leading cause. Heavy alcohol consumption, especially when combined with tobacco use, dramatically increases the risk. The human papillomavirus (HPV) infection, particularly HPV-16, is a growing cause of base of tongue cancers. Poor oral hygiene, chronic irritation from ill-fitting dentures or jagged teeth, and a diet low in fruits and vegetables can also contribute to risk. Prolonged exposure to sunlight is a risk factor for lip cancer, which can sometimes extend to the oral tongue.
Genetic Predisposition
While lifestyle and environmental factors account for the majority of tongue cancer cases, a small percentage may involve a genetic predisposition. Individuals with certain inherited genetic syndromes, such as Fanconi anemia or dyskeratosis congenita, have an increased risk of developing various cancers, including oral cancers. However, for most people, genetic factors play a less significant role compared to modifiable lifestyle risks. Family history of head and neck cancers can also slightly elevate an individual’s risk, suggesting a potential genetic component or shared environmental exposures.
Diagnosing and Treating Tongue Cancer
An accurate and timely diagnosis is the first step in managing tongue cancer, followed by a personalized treatment plan. Knowing how is tongue cancer diagnosed and the available tongue cancer treatment options is crucial for patients and their families.
Diagnostic Procedures
The diagnostic process typically begins with a thorough physical examination of the mouth and neck by a dentist or doctor. If a suspicious area is found, a biopsy is performed, where a small tissue sample is taken from the lesion and examined under a microscope by a pathologist to confirm the presence of cancer. If cancer is confirmed, further imaging tests are conducted to determine the extent (stage) of the cancer. These may include computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans. These scans help identify if the cancer has spread to lymph nodes or other parts of the body, which is critical for planning the most effective treatment strategy.
Overview of Treatment Modalities
The choice of tongue cancer treatment options depends on several factors, including the cancer’s stage, location, the patient’s overall health, and personal preferences. Common treatment modalities include:
- Surgery: Often the primary treatment, involving the removal of the tumor and a margin of healthy tissue. For larger tumors, a partial or total glossectomy (removal of part or all of the tongue) may be necessary. Lymph nodes in the neck may also be removed if there’s a risk of spread.
- Radiation Therapy: Uses high-energy rays to kill cancer cells. It can be used alone for early-stage cancers, after surgery to eliminate remaining cancer cells, or in combination with chemotherapy for more advanced cases.
- Chemotherapy: Uses drugs to kill cancer cells throughout the body. It is often used in conjunction with radiation therapy (chemoradiation) for advanced cancers or to treat cancer that has spread.
- Targeted Therapy: Drugs that specifically target cancer cells by interfering with their growth and spread, often with fewer side effects than traditional chemotherapy.
- Immunotherapy: Helps the body’s immune system fight cancer. It may be an option for advanced or recurrent tongue cancer that has not responded to other treatments.
A multidisciplinary team of specialists, including surgeons, oncologists, radiation oncologists, and supportive care professionals, typically collaborates to develop the most appropriate treatment plan.
Tongue Cancer Prognosis and Outlook
Understanding the tongue cancer prognosis is a natural concern for patients and their families. The outlook for individuals with tongue cancer varies significantly based on several key factors, highlighting the importance of early detection and comprehensive care.
Factors Influencing Outlook
The most critical factor influencing tongue cancer prognosis is the stage of the cancer at diagnosis. Cancers detected at an early stage, when they are small and confined to the tongue, generally have a much better prognosis than those diagnosed at later stages, where the cancer has spread to lymph nodes or distant sites. Other important factors include the tumor’s size and location, whether it has invaded surrounding tissues, the presence of HPV infection (which can sometimes indicate a better response to treatment for base of tongue cancers), the patient’s overall health, and their response to treatment. According to the American Cancer Society, the 5-year survival rate for localized oral cavity and pharynx cancer is approximately 84%, but this drops significantly if the cancer has spread regionally or distantly.
Importance of Follow-Up Care
After completing initial treatment, regular and rigorous follow-up care is essential. This involves frequent check-ups with the oncology team to monitor for any signs of recurrence, manage long-term side effects of treatment, and address any rehabilitation needs, such as speech therapy or swallowing therapy. Follow-up care also includes counseling on lifestyle modifications, such as quitting tobacco and reducing alcohol consumption, to minimize the risk of new primary cancers. Adherence to follow-up schedules significantly contributes to a better long-term outlook and quality of life for individuals who have undergone treatment for tongue cancer.
The most common early signs of tongue cancer include a persistent sore or ulcer on the tongue that does not heal within two weeks. Other key indicators are unexplained red or white patches (erythroplakia or leukoplakia), a persistent lump or thickening on the tongue, or a feeling of numbness in part of the tongue. Any unexplained bleeding from the tongue or persistent pain should also prompt a medical evaluation, as early detection significantly improves treatment outcomes.
Tongue cancer treatment options are tailored to the individual’s specific case, primarily based on the cancer’s stage and location. Common treatments include surgery to remove the tumor, which may involve a partial or total glossectomy. Radiation therapy uses high-energy rays to kill cancer cells, often used after surgery or in combination with chemotherapy. Chemotherapy employs drugs to destroy cancer cells, particularly for advanced or metastatic disease. Targeted therapy and immunotherapy are also emerging options, offering more precise approaches to treatment.
While not all cases of tongue cancer are preventable, a significant number can be avoided by addressing key risk factors. The most effective prevention strategies involve avoiding all forms of tobacco use and limiting alcohol consumption. Vaccination against Human Papillomavirus (HPV) can prevent HPV-related base of tongue cancers. Maintaining good oral hygiene, having regular dental check-ups, and adopting a diet rich in fruits and vegetables also contribute to reducing the risk of developing tongue cancer.