Key Takeaways
- Myelofibrosis is a rare bone marrow disorder where scar tissue replaces normal blood-forming cells.
- Symptoms often include fatigue, an enlarged spleen, anemia, and bone pain, driven by ineffective blood cell production.
- Diagnosis relies on bone marrow biopsy, blood tests, and genetic analysis for mutations like JAK2, CALR, or MPL.
- Treatment ranges from watchful waiting and supportive care to targeted therapies (JAK inhibitors) and, in some cases, stem cell transplantation.
- Ongoing research is exploring new therapeutic targets and personalized medicine approaches to improve prognosis and quality of life.
What is Myelofibrosis? Causes and Symptoms
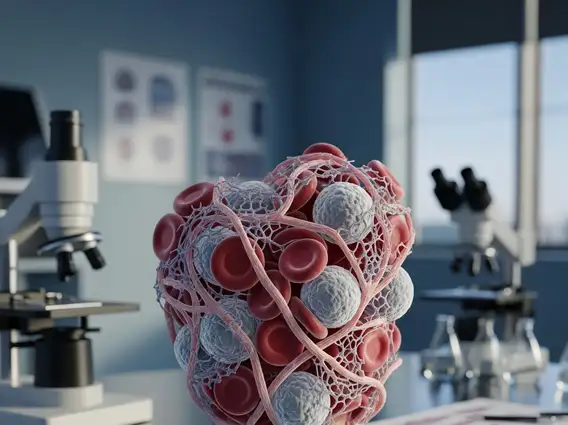
Myelofibrosis disease is a type of chronic myeloproliferative neoplasm (MPN) characterized by the progressive scarring (fibrosis) of the bone marrow. This scarring impairs the bone marrow’s ability to produce healthy blood cells, leading to a shortage of red blood cells (anemia), white blood cells, and platelets. As a result, the body attempts to produce blood cells in other organs, such as the spleen and liver, causing them to enlarge.
The exact causes of myelofibrosis explained often involve specific genetic mutations in hematopoietic stem cells. The most common mutations include Janus kinase 2 (JAK2), calreticulin (CALR), and myeloproliferative leukemia virus oncogene (MPL). These mutations lead to overactive signaling pathways that drive abnormal cell growth and the subsequent development of fibrosis in the bone marrow. While these genetic changes are acquired during a person’s lifetime and are not inherited, the precise triggers for these mutations remain largely unknown. Myelofibrosis can be primary (idiopathic) or secondary, developing from other MPNs like essential thrombocythemia or polycythemia vera.
The myelofibrosis symptoms and signs can vary widely among individuals and often develop gradually. They are primarily a result of ineffective blood cell production and an enlarged spleen. Common symptoms include:
- Fatigue and Weakness: Often due to anemia, a reduction in healthy red blood cells.
- Splenomegaly: An enlarged spleen, which can cause abdominal discomfort, pain, or a feeling of fullness after eating small amounts.
- Bone Pain: Resulting from the abnormal bone marrow activity.
- Night Sweats and Fever: Systemic symptoms often associated with chronic inflammation.
- Unexplained Weight Loss: A common constitutional symptom.
- Easy Bleeding or Bruising: Due to low platelet counts or dysfunctional platelets.
- Frequent Infections: Caused by a deficiency in functional white blood cells.
Diagnosis and Management Approaches
The process of determining how is myelofibrosis diagnosed involves a comprehensive evaluation, including physical examination, blood tests, and a bone marrow biopsy. Blood tests typically reveal anemia, abnormal white blood cell counts, and platelet counts that can be high, low, or normal. A peripheral blood smear may show characteristic tear-drop shaped red blood cells (poikilocytosis) and immature blood cells. Genetic testing is crucial to identify common mutations such as JAK2, CALR, or MPL, which help confirm the diagnosis and inform prognosis.
A bone marrow biopsy is the definitive diagnostic tool. It involves taking a small sample of bone marrow, usually from the hip bone, to examine under a microscope. This allows pathologists to assess the degree of fibrosis, the cellularity of the marrow, and the presence of abnormal cells. The findings from the biopsy, combined with blood test results and genetic analysis, are essential for distinguishing myelofibrosis from other bone marrow disorders and for accurate staging.
Myelofibrosis Treatment Options Overview
The selection of myelofibrosis treatment options overview depends on several factors, including the patient’s age, symptoms, disease stage, and genetic mutations. For some patients with low-risk disease and minimal symptoms, a “watch and wait” approach may be adopted, with regular monitoring. For those requiring intervention, treatments aim to manage symptoms, slow disease progression, and improve quality of life.
One of the primary therapeutic strategies involves Janus kinase (JAK) inhibitors, such as ruxolitinib and fedratinib. These medications target the overactive JAK-STAT signaling pathway, which is often driven by the common genetic mutations in myelofibrosis. JAK inhibitors can effectively reduce spleen size, alleviate constitutional symptoms like fatigue, night sweats, and itching, and improve overall quality of life. They do not cure the disease but can significantly manage its manifestations. Other supportive care measures include blood transfusions for severe anemia, erythropoiesis-stimulating agents, and sometimes splenectomy (surgical removal of the spleen) or radiation therapy to manage an enlarged spleen.
For a select group of eligible patients, allogeneic stem cell transplantation (SCT) is the only potentially curative treatment for myelofibrosis. This procedure involves replacing the diseased bone marrow with healthy stem cells from a donor. However, SCT is a high-risk procedure with significant potential side effects and is typically reserved for younger patients with higher-risk disease who have a suitable donor. Decisions regarding SCT are made after careful consideration of the patient’s overall health, disease characteristics, and potential risks versus benefits.
Living with the Condition: Prognosis and Outlook
The myelofibrosis prognosis and outlook can vary significantly among individuals, influenced by factors such as age at diagnosis, specific genetic mutations, blood counts, and the presence of constitutional symptoms. While myelofibrosis is a chronic and progressive condition, advancements in treatment have improved symptom management and, in some cases, extended life expectancy. Risk stratification models, such as the Dynamic International Prognostic Scoring System (DIPSS), help clinicians assess individual patient risk and guide treatment decisions.
Patients with myelofibrosis face potential complications, including severe anemia, recurrent infections due to impaired immune function, and bleeding problems. A significant concern is the risk of transformation to acute myeloid leukemia (AML), a more aggressive form of blood cancer, which occurs in a notable percentage of patients. Regular monitoring by a hematologist is essential to track disease progression, manage symptoms, and address complications promptly. Many patients learn to manage their condition effectively, maintaining a reasonable quality of life with appropriate medical care and supportive therapies.
Advancements in Research
The latest research on myelofibrosis is continually expanding our understanding of this complex disease and leading to the development of novel therapeutic strategies. Researchers are investigating new drug targets beyond the JAK-STAT pathway, exploring agents that can directly reduce bone marrow fibrosis or target specific genetic abnormalities. Clinical trials are ongoing, evaluating new JAK inhibitors, combination therapies, and drugs that modulate the immune system or epigenetic pathways.
Efforts are also focused on improving diagnostic accuracy and developing more precise prognostic markers, including advanced genetic sequencing techniques. The goal is to move towards more personalized medicine approaches, tailoring treatments based on an individual patient’s unique genetic profile and disease characteristics. These ongoing research initiatives offer hope for more effective and less toxic treatments, ultimately aiming to improve the long-term outlook and quality of life for individuals living with myelofibrosis.
Life expectancy for individuals with myelofibrosis varies greatly, depending on factors such as age, specific genetic mutations, blood counts, and symptom severity. While it is a chronic and progressive condition, advancements in treatment, particularly with JAK inhibitors, have improved symptom control and, in some cases, extended survival. Prognostic scoring systems help doctors estimate individual outlooks, but each patient’s journey is unique, and ongoing research continues to improve outcomes.
Currently, the only potential cure for myelofibrosis is an allogeneic stem cell transplant. However, this procedure is associated with significant risks and is typically reserved for younger, higher-risk patients who have a suitable donor. For most patients, treatment focuses on managing symptoms, slowing disease progression, and improving quality of life through medications like JAK inhibitors and supportive care. Research is ongoing to find less toxic and more widely applicable curative therapies.
While diet and lifestyle changes cannot cure myelofibrosis, they can play a supportive role in managing symptoms and improving overall well-being. Maintaining a balanced diet rich in nutrients, staying hydrated, and engaging in light to moderate exercise (as tolerated) can help combat fatigue and maintain muscle strength. Avoiding alcohol and tobacco is generally recommended. It’s crucial to discuss any dietary or lifestyle modifications with your healthcare provider to ensure they are safe and appropriate for your specific condition.