Key Takeaways
- Hypopharyngeal cancer develops in the lower part of the throat, often presenting with symptoms like difficulty swallowing or a persistent sore throat.
- Major risk factors include long-term tobacco and alcohol use, with HPV infection also playing a role in some cases.
- Diagnosis typically involves endoscopy, biopsy, and advanced imaging, followed by staging to determine the cancer’s extent.
- Treatment options vary based on the cancer’s stage and may include surgery, radiation therapy, chemotherapy, or a combination of these.
- Early detection significantly improves the hypopharyngeal cancer prognosis, emphasizing the importance of recognizing symptoms and seeking timely medical attention.
What is Hypopharyngeal Cancer?
Hypopharyngeal cancer refers to malignant growths that form in the hypopharynx, the lowest section of the pharynx (throat). This critical area connects the oropharynx (middle part of the throat) to the esophagus (food pipe) and the larynx (voice box), making its health vital for swallowing, breathing, and speaking. Understanding what is hypopharyngeal cancer involves recognizing its anatomical origin and cellular characteristics.
Anatomy of the Hypopharynx
The hypopharynx is a funnel-shaped structure situated behind the larynx, extending from the epiglottis down to the entrance of the esophagus. It comprises three main subsites: the piriform sinuses (two pockets on either side of the larynx), the postcricoid area (the back surface of the cricoid cartilage), and the posterior pharyngeal wall (the back wall of the throat). Cancers originating here can quickly affect nearby structures, including the vocal cords and lymph nodes in the neck, due to the rich lymphatic drainage of the region.
Types of Hypopharyngeal Cancer
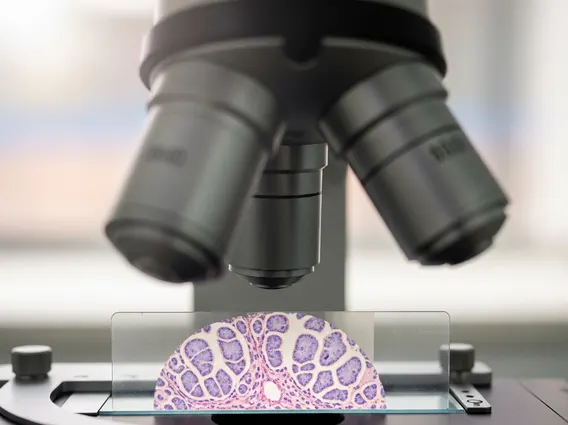
The vast majority of hypopharyngeal cancers, approximately 95%, are squamous cell carcinomas. These cancers develop from the flat, thin cells that line the moist surfaces inside the hypopharynx. Rarer types include sarcomas, lymphomas, and adenocarcinomas, but these are far less common. The specific type of cancer influences its growth pattern, potential for spread, and responsiveness to various treatments.
Symptoms and Risk Factors
Recognizing the signs and understanding the factors that contribute to the development of hypopharyngeal cancer is crucial for early detection and prevention. Many symptoms can be subtle initially, often mimicking less serious conditions, which can delay diagnosis.
Common Warning Signs
The hypopharyngeal cancer symptoms often become noticeable as the tumor grows and begins to interfere with normal functions. These can include:
- Dysphagia (Difficulty Swallowing): This is one of the most common symptoms, often starting as a feeling of food getting stuck in the throat or pain during swallowing.
- Voice Changes: Hoarseness or a change in voice quality can occur if the tumor affects the vocal cords or nerves controlling them.
- Persistent Sore Throat or Ear Pain: A chronic sore throat that does not resolve, especially if accompanied by pain radiating to the ear (otalgia), can be a warning sign.
- Lump in the Neck: Swelling or a palpable mass in the neck, often due to enlarged lymph nodes where cancer cells have spread, is a significant indicator.
- Unexplained Weight Loss: Significant weight loss without intentional dieting can be a symptom of advanced cancer.
- Difficulty Breathing: In later stages, a large tumor can obstruct the airway, leading to shortness of breath or noisy breathing.
It is important to note that these symptoms can also be caused by other conditions, but their persistence warrants medical evaluation.
Key Causes and Lifestyle Risks
The causes of hypopharyngeal cancer are primarily linked to certain lifestyle choices and environmental exposures. The most significant risk factors include:
- Tobacco Use: Smoking cigarettes, cigars, pipes, and using smokeless tobacco products dramatically increases the risk. The chemicals in tobacco damage the cells lining the throat.
- Alcohol Consumption: Heavy and prolonged alcohol use is a major risk factor. The combination of tobacco and alcohol use multiplies the risk significantly more than either factor alone.
- Human Papillomavirus (HPV) Infection: Certain high-risk strains of HPV, particularly HPV-16, are increasingly recognized as a cause of head and neck cancers, including some hypopharyngeal cancers.
- Poor Nutrition: Diets lacking in fruits and vegetables may increase susceptibility.
- Plummer-Vinson Syndrome: This rare condition, characterized by iron deficiency anemia, difficulty swallowing, and esophageal webs, is associated with an increased risk of postcricoid hypopharyngeal cancer.
Avoiding these risk factors is the most effective way to prevent the development of hypopharyngeal cancer.
Diagnosis and Staging
Accurate hypopharyngeal cancer diagnosis and precise staging are critical steps in determining the most effective treatment plan. The diagnostic process involves a series of examinations and tests to confirm the presence of cancer and assess its extent.
Diagnostic Procedures
When symptoms suggest hypopharyngeal cancer, a doctor will typically perform several diagnostic procedures:
- Physical Examination: A thorough examination of the head and neck, including palpation for lumps and swollen lymph nodes.
- Indirect Laryngoscopy/Pharyngoscopy: Using a small mirror and light or a flexible fiber-optic scope (endoscope) to visualize the hypopharynx and surrounding areas.
- Direct Laryngoscopy/Pharyngoscopy and Biopsy: Performed under general anesthesia, this allows for a more detailed examination and the collection of tissue samples (biopsy) from any suspicious areas. The biopsy is then examined under a microscope to confirm cancer.
- Imaging Tests:
- CT (Computed Tomography) Scan: Provides detailed cross-sectional images to show the tumor’s size, location, and spread to nearby tissues or lymph nodes.
- MRI (Magnetic Resonance Imaging): Offers excellent soft tissue contrast, useful for assessing tumor invasion into muscles, nerves, and blood vessels.
- PET (Positron Emission Tomography) Scan: Helps identify active cancer cells throughout the body, useful for detecting distant metastases.
Understanding Cancer Stages
Once cancer is confirmed, it is staged to describe its size, location, and whether it has spread. The stages of hypopharyngeal cancer typically range from Stage 0 to Stage IV, with higher numbers indicating more advanced disease:
| Stage | Description |
|---|---|
| Stage 0 (Carcinoma in Situ) | Abnormal cells are present only in the lining of the hypopharynx and have not invaded deeper tissues. |
| Stage I | The tumor is small (2 cm or less) and has not spread to lymph nodes or distant sites. |
| Stage II | The tumor is larger (more than 2 cm but not more than 4 cm) or has spread to one lymph node on the same side as the tumor, but the node is not larger than 3 cm. |
| Stage III | The tumor is larger than 4 cm, or has spread to one lymph node on the same side (not larger than 6 cm), or to multiple lymph nodes on the same side (none larger than 6 cm), or to one lymph node on the opposite side (not larger than 6 cm). |
| Stage IV | The cancer has spread to nearby structures (e.g., bone, cartilage), or to larger or more distant lymph nodes, or to distant parts of the body (metastasis). |
Staging is a crucial factor in determining the hypopharyngeal cancer treatment options and predicting the patient’s prognosis.
Hypopharyngeal Cancer Treatment
The approach to treating hypopharyngeal cancer is highly individualized, depending on the cancer’s stage, location, the patient’s overall health, and personal preferences. A multidisciplinary team of specialists typically collaborates to develop the most effective strategy, which often involves a combination of therapies.
Surgical Interventions
Surgery is a common component of hypopharyngeal cancer treatment options, especially for early-stage disease. The goal is to remove the tumor and a margin of healthy tissue. Surgical procedures may include:
- Partial Pharyngectomy: Removal of only the cancerous part of the hypopharynx, preserving as much function as possible.
- Total Pharyngectomy: Removal of the entire hypopharynx, often necessary for larger tumors. This procedure typically requires reconstructive surgery.
- Laryngopharyngectomy: If the cancer has spread to the larynx, both the larynx and part or all of the hypopharynx may need to be removed. This results in permanent loss of the voice box and requires a tracheostomy.
- Neck Dissection: Removal of lymph nodes in the neck if cancer cells are suspected or confirmed to have spread to them.
Reconstructive surgery often follows extensive resections to restore swallowing and speech functions, using tissue from other parts of the body.
Radiation and Chemotherapy
These therapies are frequently used either alone, in combination with each other, or as adjuncts to surgery:
- Radiation Therapy: Uses high-energy X-rays or other particles to kill cancer cells or inhibit their growth. It can be used as the primary treatment for early-stage cancers, after surgery to eliminate any remaining cancer cells (adjuvant therapy), or to alleviate symptoms in advanced cases. Techniques like Intensity-Modulated Radiation Therapy (IMRT) help target tumors more precisely, reducing damage to surrounding healthy tissues.
- Chemotherapy: Involves drugs that kill cancer cells throughout the body. It is often given in combination with radiation therapy (chemoradiation) to enhance its effectiveness, especially for more advanced cancers or to shrink tumors before surgery. Chemotherapy can also be used to treat metastatic disease.
- Targeted Therapy: These drugs specifically target certain molecules involved in cancer growth and spread, often with fewer side effects than traditional chemotherapy.
- Immunotherapy: Utilizes the body’s own immune system to fight cancer. Drugs called checkpoint inhibitors can be used for recurrent or metastatic hypopharyngeal cancer that has not responded to other treatments.
The choice of treatment is a complex decision, weighing the potential benefits against the possible side effects and impact on quality of life.
Prognosis and Recovery
Understanding the hypopharyngeal cancer prognosis and the recovery process is vital for patients and their families. The outlook can vary significantly based on several factors, and life after treatment often involves a comprehensive rehabilitation plan.
Factors Influencing Outlook
The prognosis for hypopharyngeal cancer is influenced by several key factors:
- Stage at Diagnosis: This is the most critical factor. Cancers diagnosed at earlier stages (Stage I or II) generally have a much better prognosis than those found at later stages (Stage III or IV) when the cancer has spread.
- Tumor Location and Size: Tumors in certain subsites of the hypopharynx or larger tumors may be more challenging to treat effectively.
- Lymph Node Involvement: The presence and extent of cancer spread to regional lymph nodes significantly worsen the prognosis.
- Overall Health and Age: Patients who are in good general health and younger tend to tolerate treatment better and may have a more favorable outcome.
- Response to Treatment: How well the cancer responds to initial therapy plays a crucial role in long-term survival.
- HPV Status: For some head and neck cancers, HPV-positive tumors may have a better prognosis and respond differently to treatment compared to HPV-negative tumors, though this link is more established for oropharyngeal cancers.
According to the American Cancer Society, the 5-year survival rates for hypopharyngeal cancer vary significantly by stage: approximately 58% for localized disease, 33% for regional spread, and 18% for distant metastasis. These statistics highlight the importance of early detection and comprehensive treatment strategies.
Life After Treatment
Recovery from hypopharyngeal cancer treatment is a multifaceted process that often requires significant support and rehabilitation. Patients may face challenges related to:
- Speech and Swallowing: Surgery and radiation can impact the ability to speak and swallow. Speech-language pathologists play a crucial role in helping patients regain these functions through exercises and adaptive techniques.
- Nutrition: Difficulty swallowing may necessitate dietary modifications, nutritional supplements, or even a feeding tube (gastrostomy tube) temporarily or permanently.
- Psychological Support: Dealing with cancer and its aftermath can be emotionally challenging. Support groups, counseling, and psychological therapy can be invaluable.
- Follow-up Care: Regular follow-up appointments with the oncology team are essential to monitor for recurrence, manage side effects, and ensure overall well-being. This typically involves physical exams and imaging tests.
- Lifestyle Adjustments: Quitting tobacco and alcohol use is critical for preventing recurrence and improving overall health.
A comprehensive rehabilitation plan, tailored to individual needs, is key to improving the quality of life for survivors of hypopharyngeal cancer.
Early signs of hypopharyngeal cancer can be subtle and often include persistent difficulty or pain when swallowing (dysphagia), a chronic sore throat that doesn’t improve, or a noticeable change in voice quality, such as hoarseness. Some individuals might also experience ear pain that radiates from the throat. Any of these symptoms, especially if they persist for more than a few weeks, warrant prompt medical evaluation to rule out serious conditions and ensure timely diagnosis.
Prevention of hypopharyngeal cancer primarily involves avoiding key risk factors. The most effective strategies include refraining from all forms of tobacco use, including smoking and smokeless products, and limiting or avoiding alcohol consumption. Maintaining a healthy diet rich in fruits and vegetables can also contribute to prevention. Additionally, vaccination against Human Papillomavirus (HPV) may help reduce the risk of HPV-related head and neck cancers, though its direct impact on hypopharyngeal cancer is still being studied.
The recovery time after hypopharyngeal cancer treatment varies significantly depending on the stage of cancer, the specific treatments received (surgery, radiation, chemotherapy), and the individual’s overall health. Surgical recovery can take several weeks to months, especially if reconstructive surgery is involved. Radiation and chemotherapy side effects can persist for weeks or months after treatment concludes. Full recovery, including rehabilitation for speech and swallowing, can be a long-term process, often requiring ongoing therapy and support for up to a year or more.