Key Takeaways
- Muscle weakness can stem from diverse origins, including neurological conditions, muscular diseases, systemic illnesses, and lifestyle factors.
- Muscle Weakness in cancer patients is a significant concern, often resulting from the disease itself, its treatments, or associated conditions like cachexia.
- Recognizing symptoms of muscle weakness such as difficulty with movement, fatigue, or balance issues is vital for early intervention.
- Accurate muscle weakness diagnosis involves a comprehensive medical history, physical examination, and various diagnostic tests.
- Effective management includes addressing the underlying cause, physical therapy, nutritional support, and targeted exercises for muscle weakness.
Causes of Muscle Weakness & Cancer Patient Impact
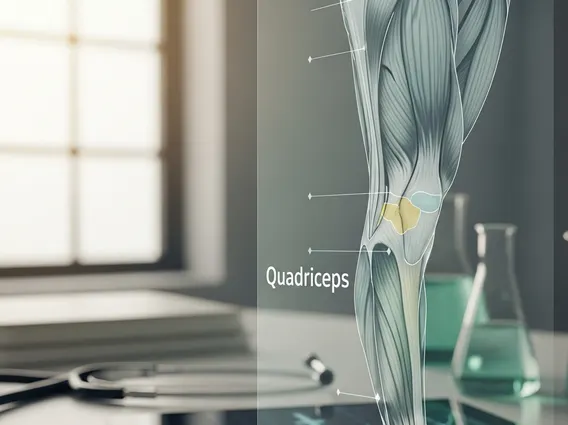
Understanding what causes muscle weakness is the first step toward effective management. This complex symptom can arise from a multitude of factors affecting the nervous system, muscles themselves, or overall bodily functions. Common causes include neurological disorders such as stroke, multiple sclerosis, or peripheral neuropathy, which disrupt nerve signals to muscles. Muscular diseases like muscular dystrophy or myositis directly impair muscle fibers. Additionally, systemic conditions such as thyroid disorders, kidney disease, or severe infections can lead to generalized weakness.
A particularly significant area of concern is Muscle Weakness in cancer patients. Cancer and its treatments frequently induce profound weakness, often manifesting as cancer-related fatigue (CRF) or cachexia. Cancer cachexia, a complex metabolic syndrome, leads to involuntary weight loss, muscle wasting, and decreased physical function, severely impacting strength. Chemotherapy, radiation therapy, and immunotherapy can also cause muscle damage, neuropathy, or systemic inflammation, contributing to weakness. According to the National Cancer Institute, cancer-related fatigue, which often includes muscle weakness, affects up to 90% of cancer patients, significantly diminishing their quality of life and treatment adherence.
Specific patterns of weakness can also point to particular causes. For instance, muscle weakness in legs causes can range from common issues like prolonged immobility or electrolyte imbalances to more serious conditions such as lumbar spinal stenosis, peripheral artery disease, or diabetic neuropathy. These conditions can restrict blood flow, compress nerves, or damage nerve fibers, leading to a noticeable reduction in leg strength and mobility. Identifying the precise cause is paramount for tailoring appropriate interventions and improving patient outcomes.
Identifying Muscle Weakness: Symptoms & Diagnosis
Recognizing the symptoms of muscle weakness is crucial for early intervention and effective treatment. These symptoms can vary widely depending on the underlying cause, the specific muscles affected, and the severity of the condition. While some individuals may experience a generalized feeling of fatigue and overall body weakness, others might notice weakness localized to specific limbs or muscle groups. Prompt identification allows for a timely medical evaluation, which is essential for preventing further complications and improving the prognosis.
The process of muscle weakness diagnosis typically begins with a thorough medical history and a comprehensive physical examination. During the physical exam, a doctor will assess muscle strength, reflexes, coordination, and sensation. They will look for signs of muscle atrophy (wasting) or fasciculations (small, involuntary muscle twitches). The physician will also inquire about the onset, progression, and any associated symptoms, such as pain, numbness, or difficulty with specific movements. This initial assessment helps to narrow down the potential causes and guide further diagnostic testing.
Recognizing the Signs
The manifestations of muscle weakness can significantly impact daily life. It’s important to be aware of the various ways it can present itself. Common symptoms of muscle weakness include:
- Difficulty lifting objects or performing tasks that once felt easy.
- Trouble standing up from a seated position or climbing stairs.
- Frequent falls or a sensation of instability and loss of balance.
- Muscle cramps, spasms, or tremors that accompany the weakness.
- Fatigue that doesn’t improve with rest, often disproportionate to activity levels.
- Changes in gait or walking patterns, such as dragging feet.
- Difficulty with fine motor skills, like buttoning clothes or writing.
- Shortness of breath or difficulty swallowing in severe cases affecting respiratory or throat muscles.
If you experience any of these persistent symptoms, especially if they worsen over time or appear suddenly, seeking medical advice is important to determine the underlying cause and receive appropriate care.
Diagnostic Procedures
To pinpoint the exact cause of muscle weakness, a doctor may order a range of diagnostic tests. These tests help to evaluate nerve function, muscle health, and systemic conditions. Common diagnostic procedures include:
| Test Type | Purpose | What it Measures |
|---|---|---|
| Blood Tests | Identify systemic causes | Electrolyte imbalances, thyroid hormones, inflammatory markers, vitamin deficiencies, kidney/liver function, specific antibodies. |
| Electromyography (EMG) | Assess muscle electrical activity | Electrical potential generated by muscle cells when activated by nerves, detecting nerve or muscle damage. |
| Nerve Conduction Studies (NCS) | Evaluate nerve function | Speed and strength of signals traveling along nerves, identifying nerve damage or compression. |
| Magnetic Resonance Imaging (MRI) | Visualize soft tissues | Detailed images of brain, spinal cord, and muscles to detect structural abnormalities, tumors, or inflammation. |
| Muscle Biopsy | Examine muscle tissue | Microscopic analysis of a small muscle sample to identify specific muscle diseases or inflammatory conditions. |
These diagnostic tools provide critical information that helps healthcare providers formulate an accurate diagnosis and develop a targeted treatment plan for the specific type of muscle weakness identified.
Effective Treatments & Exercises for Muscle Weakness
Addressing how to treat muscle weakness effectively involves a multi-faceted approach that targets the underlying cause while also managing symptoms and improving functional strength. Treatment plans are highly individualized, depending on the specific diagnosis, the severity of weakness, and the patient’s overall health. For instance, if the weakness is due to an infection, antibiotics may be prescribed. If it stems from a nutritional deficiency, dietary changes or supplements will be recommended. In cases of autoimmune conditions, immunosuppressants might be necessary to reduce inflammation and prevent further muscle damage.
Physical therapy plays a pivotal role in the recovery and management of muscle weakness. Therapists design customized programs to strengthen weakened muscles, improve range of motion, enhance balance, and restore functional independence. Occupational therapy can also assist individuals in adapting to daily tasks and using assistive devices if necessary. Nutritional support is often critical, especially for conditions like cancer cachexia, where adequate protein and calorie intake are essential to combat muscle wasting. Medications may also be used to manage symptoms such as pain or muscle spasms, further facilitating rehabilitation efforts.
Incorporating specific exercises for muscle weakness is fundamental to regaining strength and mobility. The types of muscle weakness, whether generalized or localized, acute or chronic, will dictate the most appropriate exercise regimen. For example, progressive resistance training is highly effective for building muscle mass and strength, while flexibility exercises can improve range of motion and prevent stiffness. Balance exercises are crucial for reducing the risk of falls, particularly for individuals experiencing weakness in their legs. It is important that all exercise programs are supervised by a healthcare professional or physical therapist to ensure safety and effectiveness, preventing injury and optimizing outcomes.
For individuals experiencing chronic or severe weakness, such as those with neurological conditions or advanced cancer, the focus of treatment may shift towards maintaining existing strength, preventing further decline, and improving comfort and quality of life. This can involve adaptive equipment, energy conservation techniques, and ongoing supportive care. Regular monitoring and adjustments to the treatment plan are essential to respond to changes in the patient’s condition and ensure the most beneficial approach.
No, muscle weakness is not always serious. It can sometimes be a temporary symptom of fatigue, minor illness, or overexertion, resolving with rest. However, persistent, unexplained, or worsening muscle weakness can indicate an underlying medical condition ranging from nutritional deficiencies to more serious neurological or muscular disorders. It’s crucial to consult a healthcare professional if muscle weakness is new, severe, or accompanied by other concerning symptoms to determine its cause and appropriate treatment.
Yes, diet can significantly influence muscle strength and overall energy levels. Adequate intake of protein is essential for muscle repair and growth, while carbohydrates provide energy for muscle function. Vitamins and minerals, such as Vitamin D, magnesium, and potassium, also play crucial roles in muscle health and nerve signaling. Dehydration can exacerbate weakness, so proper hydration is vital. A balanced diet rich in whole foods can support muscle health and may help alleviate certain types of weakness, especially those related to nutritional deficiencies.
The recovery time for muscle weakness varies greatly depending on its underlying cause, severity, and the individual’s overall health. For temporary weakness due to fatigue or minor illness, recovery might be quick, within days. For more complex causes like stroke or severe injury, recovery can take weeks, months, or even longer, often requiring extensive physical therapy and rehabilitation. Chronic conditions may involve ongoing management rather than a complete “recovery.” Consistency with treatment and rehabilitation is key to optimizing outcomes.