Prostatitis
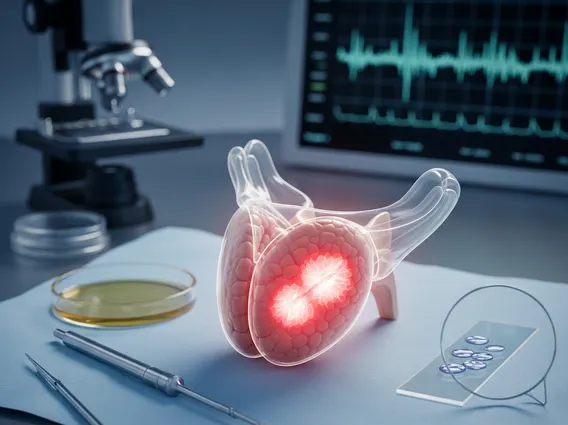
Prostatitis is a common and often painful condition involving inflammation of the prostate gland, a walnut-sized gland located just below the bladder in men. This article will explore its various forms, common symptoms, underlying causes, and available treatment strategies to help you understand this condition better.
Key Takeaways
- Prostatitis refers to the inflammation of the prostate gland, affecting men of all ages.
- It manifests in several forms: acute bacterial, chronic bacterial, chronic pelvic pain syndrome (CPPS), and asymptomatic inflammatory prostatitis.
- Common symptoms include pelvic pain, urinary difficulties, and discomfort during ejaculation.
- Causes vary by type, ranging from bacterial infections to nerve issues or psychological stress.
- Treatment is tailored to the specific type and may involve antibiotics, anti-inflammatory drugs, or lifestyle modifications.
What is Prostatitis?
Prostatitis is a medical condition characterized by inflammation of the prostate gland. This gland plays a vital role in the male reproductive system, producing seminal fluid that nourishes and transports sperm. While it can affect men of any age, it is particularly common in men under 50, making it one of the most frequently diagnosed urological conditions in this age group. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), prostatitis accounts for approximately 2 million doctor visits per year in the United States. The condition can significantly impact a man’s quality of life due to its often debilitating symptoms.
Types, Symptoms, and Causes of Prostatitis
Understanding the different types of prostatitis is crucial for accurate diagnosis and effective treatment, as each type has distinct characteristics regarding its onset, duration, and underlying causes. The primary types include acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome (CPPS), and asymptomatic inflammatory prostatitis. Each type presents with varying degrees of discomfort and specific diagnostic indicators.
Common Prostatitis symptoms and causes often overlap but can also be unique to each type:
- Acute Bacterial Prostatitis: This is a severe, sudden bacterial infection of the prostate. Symptoms include fever, chills, body aches, nausea, vomiting, frequent urination, painful urination (dysuria), and pain in the lower back or pelvic area. It is caused by bacterial infections, often from urinary tract infections (UTIs) that spread to the prostate.
- Chronic Bacterial Prostatitis: This involves recurrent bacterial infections of the prostate, leading to persistent or recurring urinary tract infections. Symptoms are similar to acute bacterial prostatitis but are usually less severe and develop gradually. Causes are typically persistent bacterial infections that are difficult to eradicate from the prostate tissue.
- Chronic Pelvic Pain Syndrome (CPPS): This is the most common type, characterized by pelvic pain lasting at least three months without evidence of bacterial infection. Symptoms include pain in the perineum, lower abdomen, penis, or scrotum, often accompanied by urinary urgency, frequency, and painful ejaculation. The exact causes are not fully understood but may involve nerve damage, muscle spasms, inflammation, psychological stress, or autoimmune factors.
- Asymptomatic Inflammatory Prostatitis: In this type, inflammation of the prostate is present, often detected incidentally during tests for other conditions (e.g., infertility or prostate cancer screening), but the individual experiences no symptoms. The cause is unknown, and it typically requires no treatment.
Prostatitis Treatment Options
Treatment for prostatitis is highly individualized and depends significantly on the specific type of the condition and the severity of symptoms. The goal is to alleviate pain, manage urinary symptoms, and eradicate any underlying infection. A healthcare provider will typically conduct a thorough evaluation, including physical exams, urine tests, and sometimes imaging, to determine the most appropriate course of action.
For bacterial forms of prostatitis, antibiotics are the cornerstone of treatment. Acute bacterial prostatitis requires immediate and often prolonged courses of antibiotics, typically for several weeks, to ensure the infection is fully cleared and to prevent it from becoming chronic. Chronic bacterial prostatitis also requires antibiotics, sometimes for several months, to penetrate the prostate tissue effectively. In addition to antibiotics, alpha-blockers may be prescribed to relax bladder neck muscles and improve urine flow, thereby reducing urinary symptoms.
For chronic pelvic pain syndrome (CPPS), which is not caused by bacteria, treatment focuses on symptom management. This can include anti-inflammatory drugs (NSAIDs), muscle relaxants, alpha-blockers, and sometimes nerve pain medications. Lifestyle modifications such as avoiding irritants (e.g., caffeine, spicy foods), warm baths, and stress management techniques can also be beneficial. Physical therapy, including pelvic floor exercises, may help alleviate muscle tension and pain. In some cases, alternative therapies like acupuncture or biofeedback are explored, but it is important to note that these are supportive measures and do not replace conventional medical treatment.
