Progression
Progression, in a medical context, refers to the advancement or worsening of a disease over time. Understanding this concept is crucial for diagnosis, treatment planning, and patient management across various medical disciplines.

Key Takeaways
- Progression signifies the worsening of a medical condition or disease, often indicating a need for treatment adjustment.
- It is a critical indicator for evaluating the effectiveness of therapies and guiding subsequent patient care decisions.
- Types of progression include local, regional, and distant, particularly relevant in the staging and management of cancers.
- Factors such as genetics, lifestyle choices, and adherence to treatment protocols significantly influence how a disease progresses.
- Monitoring progression helps healthcare providers make informed decisions, aiming to improve patient outcomes and quality of life.
What is Progression: Definition and Medical Context
In medicine, progression definition refers to the natural course of a disease advancing or deteriorating. This can manifest as an increase in the severity of symptoms, the growth of a tumor, or the spread of a condition to new areas of the body. The concept is central to understanding disease dynamics and is a key metric used by clinicians to assess patient status and treatment efficacy.
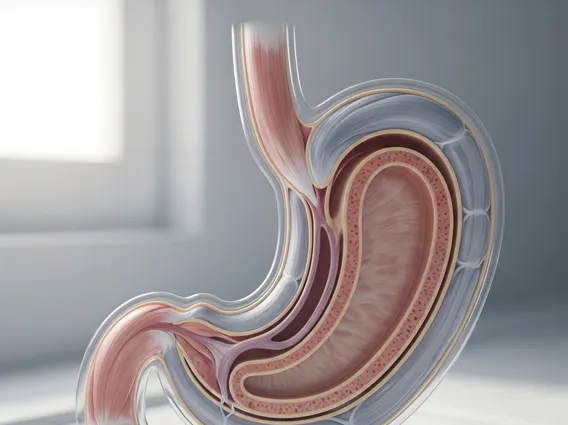
The progression meaning and examples are diverse, depending on the specific medical condition. For instance, in oncology, progression typically means that cancer is growing, spreading, or worsening, despite ongoing treatment. This could involve an increase in tumor size, the appearance of new lesions, or the spread of cancer to distant organs. In chronic diseases like multiple sclerosis, progression might involve an increase in neurological deficits or a higher frequency of relapses. Monitoring progression allows healthcare teams to adapt treatment strategies, manage symptoms more effectively, and provide appropriate supportive care.
Types of Progression in Clinical Practice
The manifestation of disease progression can vary significantly, especially in oncology, where it is often categorized based on its anatomical spread. Types of progression explained help clinicians understand the extent of disease activity and tailor interventions accordingly. These classifications are vital for accurate staging and prognosis.
Common types of progression observed in clinical practice include:
- Local Progression: The disease worsens or grows within the original site or organ where it first appeared. For example, a tumor increasing in size without spreading to surrounding tissues.
- Regional Progression: The disease spreads to nearby lymph nodes or tissues adjacent to the primary site. This indicates a more advanced stage than local progression but is still confined to a specific area of the body.
- Distant Progression (Metastasis): The disease spreads from the primary site to distant organs or tissues through the bloodstream or lymphatic system. This is often the most advanced form of progression and significantly impacts treatment options and prognosis.
- Clinical Progression: Refers to the worsening of symptoms or the appearance of new clinical signs, regardless of radiological findings. This is particularly relevant in conditions where imaging may not fully capture disease activity, such as neurodegenerative disorders.
Each type requires a distinct approach to management, highlighting the importance of precise diagnostic evaluation.
Factors Influencing Disease Progression
Many elements can influence the rate and trajectory of disease progression, making understanding the concept of progression multifaceted. These factors can be broadly categorized into host-related, disease-related, and treatment-related influences. Genetic predispositions, for example, can make individuals more susceptible to aggressive disease courses or less responsive to certain therapies.
Lifestyle choices also play a significant role. Factors such as diet, physical activity levels, smoking, and alcohol consumption can either accelerate or mitigate disease progression in conditions like cardiovascular disease, diabetes, and certain cancers. Furthermore, the inherent biology of the disease itself, including its aggressiveness and specific molecular characteristics, heavily dictates its natural history. Treatment adherence and the effectiveness of therapeutic interventions are paramount. For instance, early diagnosis and timely, effective treatment can dramatically alter the course of many diseases. According to the American Cancer Society, early detection of colorectal cancer can lead to a 90% 5-year survival rate when localized, compared to 14% once it has metastasized, highlighting the critical role of timely intervention in altering disease progression.