Pneumothorax
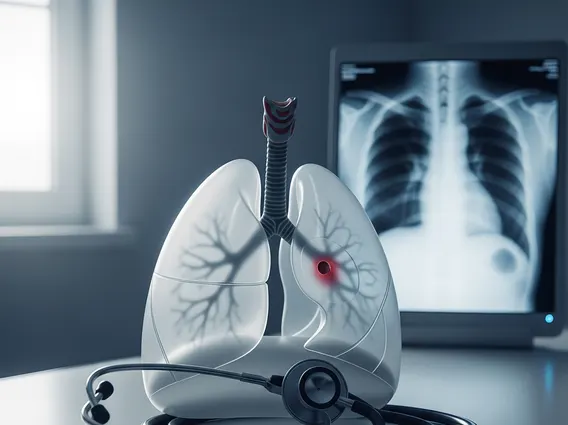
Pneumothorax, commonly known as a collapsed lung, is a serious medical condition that occurs when air leaks into the space between the lung and chest wall, causing the lung to partially or completely collapse. Understanding its causes, symptoms, and treatment is crucial for effective management.
Key Takeaways
- Pneumothorax is a collapsed lung caused by air leaking into the pleural space.
- It can result from spontaneous events, trauma, or medical procedures.
- Common symptoms include sudden chest pain and shortness of breath.
- Diagnosis typically involves physical examination and imaging like chest X-rays.
- Treatment ranges from observation to chest tube insertion or surgery, with recovery varying based on severity.
What is Pneumothorax and Its Causes
Pneumothorax refers to the presence of air in the pleural space, the area between the lung and the inner chest wall. This air buildup exerts pressure on the lung, leading to its partial or complete collapse. This condition can be life-threatening if not promptly addressed, as it impairs the lung’s ability to inflate and exchange oxygen effectively.
The causes of pneumothorax can be broadly categorized into spontaneous, traumatic, and iatrogenic:
- Spontaneous Pneumothorax: This occurs without any apparent external injury. It’s further divided into primary spontaneous pneumothorax (PSP), which happens in people without underlying lung disease (often tall, thin men who smoke), and secondary spontaneous pneumothorax (SSP), which occurs in individuals with pre-existing lung conditions such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, or asthma.
- Traumatic Pneumothorax: This type results from an injury to the chest that punctures the lung or chest wall. Common causes include rib fractures, stab wounds, gunshot wounds, or blunt force trauma from accidents.
- Iatrogenic Pneumothorax: This is a complication of medical procedures. Examples include lung biopsies, central venous catheter insertion, mechanical ventilation, or cardiopulmonary resuscitation (CPR).
According to the National Heart, Lung, and Blood Institute, primary spontaneous pneumothorax affects approximately 7.4 to 18 cases per 100,000 people per year in men and 1.2 to 6 cases per 100,000 people per year in women, highlighting its prevalence in certain demographics.
Pneumothorax Symptoms and Diagnosis
Recognizing Pneumothorax symptoms and treatment options begins with identifying the characteristic signs. The onset of symptoms is often sudden and can range from mild to severe, depending on the size of the collapsed lung and the individual’s overall health. Common symptoms include:
- Sudden, sharp chest pain on one side, which may worsen with deep breaths or coughing.
- Shortness of breath (dyspnea), which can range from mild breathlessness to severe respiratory distress.
- Rapid heart rate (tachycardia).
- Rapid breathing (tachypnea).
- A dry cough.
- Cyanosis (a bluish tinge to the skin due to lack of oxygen) in severe cases.
To determine how to diagnose a collapsed lung pneumothorax, healthcare providers typically begin with a physical examination, listening to the chest with a stethoscope for diminished or absent breath sounds on the affected side. However, definitive diagnosis relies on imaging tests. A chest X-ray is the most common and usually sufficient method to visualize the air in the pleural space and the collapsed lung. In some cases, a CT scan may be performed to provide a more detailed view, especially for smaller pneumothoraces or to identify underlying lung disease.
Treatment Options and Recovery for Pneumothorax
The approach to Pneumothorax treatment options depends on the size of the pneumothorax, its cause, the severity of symptoms, and the patient’s overall health. For very small pneumothoraces with minimal symptoms, observation may be sufficient, as the air can reabsorb on its own. Oxygen therapy may be provided to speed up air reabsorption.
More significant pneumothoraces often require intervention to remove the air from the pleural space. This can involve:
- Needle Aspiration: A small needle is inserted into the chest wall to withdraw the air.
- Chest Tube Insertion: A larger tube is inserted into the chest cavity and connected to a suction device to continuously remove air, allowing the lung to re-expand. This is a common and effective treatment.
- Surgery: For recurrent pneumothorax or cases that don’t respond to less invasive treatments, surgical procedures like pleurodesis (to make the lung adhere to the chest wall) or pleurectomy (removal of part of the pleural lining) may be performed.
The Pneumothorax recovery time and prognosis vary widely. For uncomplicated cases treated with aspiration or a chest tube, recovery can take a few days to a few weeks. Patients are typically advised to avoid strenuous activities, flying, and smoking during the recovery period. The prognosis is generally good, especially for primary spontaneous pneumothorax. However, there is a risk of recurrence, particularly for spontaneous types. Patients with underlying lung disease or those who have experienced traumatic pneumothorax may have a longer recovery period and a higher risk of complications. Regular follow-up with a healthcare provider is essential to monitor lung function and prevent recurrence.