Pneumonitis
Pneumonitis refers to a general inflammation of lung tissue, distinct from pneumonia which is typically caused by infection. This condition can arise from various irritants, exposures, or underlying medical conditions, leading to a range of respiratory symptoms.
Key Takeaways
- Pneumonitis is lung inflammation caused by non-infectious agents, differing from pneumonia.
- Symptoms often include cough, shortness of breath, and fatigue, developing acutely or chronically.
- Causes vary widely, from environmental exposures to medications and autoimmune diseases.
- Diagnosis involves a combination of medical history, imaging, and sometimes lung biopsy.
- Effective management relies on identifying and eliminating the causative agent.
What is Pneumonitis?
Pneumonitis is a broad term describing inflammation of the lung tissue, often affecting the alveoli (air sacs) and bronchioles. Unlike pneumonia, which is primarily caused by bacteria, viruses, or fungi, pneumonitis typically results from non-infectious irritants. These irritants can trigger an immune response in the lungs, leading to inflammation, scarring, and impaired lung function. According to data from the American Lung Association, interstitial lung diseases, which include many forms of pneumonitis, affect hundreds of thousands of individuals in the United States, highlighting the prevalence and impact of these conditions on respiratory health.
The condition can manifest in various forms, depending on the specific cause and the duration of exposure. It can be acute, developing rapidly after a significant exposure, or chronic, progressing slowly over months or years due to ongoing or repeated exposure to a harmful agent. Understanding the specific type and cause is crucial for effective treatment and management.
Pneumonitis Symptoms and Causes
Pneumonitis symptoms and causes are diverse, reflecting the wide array of potential triggers for lung inflammation. Symptoms can vary in severity and onset, depending on whether the condition is acute or chronic.
Common symptoms of pneumonitis include:
- Cough: Often dry, but can sometimes produce phlegm.
- Shortness of breath (dyspnea): May worsen with activity or over time.
- Fatigue: Persistent tiredness and lack of energy.
- Fever and chills: More common in acute forms.
- Chest tightness or discomfort: A feeling of pressure in the chest.
- Weight loss: Can occur in chronic cases due to ongoing inflammation and increased metabolic demand.
The causes of pneumonitis are numerous and can be broadly categorized:
| Category | Examples of Causes |
|---|---|
| Environmental/Occupational | Mold, bird droppings, chemical fumes, certain dusts (e.g., silica, asbestos) |
| Medication-induced | Chemotherapy drugs, certain antibiotics, anti-arrhythmics, biologics |
| Radiation-induced | Therapeutic radiation to the chest for cancer treatment |
| Autoimmune diseases | Rheumatoid arthritis, lupus, scleroderma, inflammatory bowel disease |
| Hypersensitivity | Repeated inhalation of allergens, leading to hypersensitivity pneumonitis |
Identifying the specific cause is paramount, as removing the offending agent is often the first and most critical step in treatment. For instance, hypersensitivity pneumonitis, a common type, results from an allergic reaction to inhaled organic dusts or chemicals.
Types and Diagnosis of Pneumonitis
The various types of pneumonitis are often classified by their cause, and accurately diagnosing pneumonitis involves a comprehensive approach to identify the specific trigger and assess the extent of lung damage.
Types of pneumonitis include hypersensitivity pneumonitis (farmer’s lung, bird fancier’s lung), chemical pneumonitis, radiation pneumonitis, drug-induced pneumonitis, and aspiration pneumonitis. Each type has distinct characteristics and often requires specific management strategies. For example, radiation pneumonitis occurs as a side effect of radiation therapy for cancers in the chest region, while aspiration pneumonitis results from inhaling gastric contents or other foreign materials into the lungs.
To diagnose pneumonitis, healthcare providers typically begin with a detailed medical history, focusing on potential exposures at home, work, or through medications. A physical examination will assess lung sounds and overall respiratory function. Diagnostic tests often include:
- Imaging studies: Chest X-rays and high-resolution computed tomography (HRCT) scans are essential to visualize lung inflammation, scarring, and specific patterns characteristic of different types of pneumonitis.
- Pulmonary function tests (PFTs): These tests measure lung capacity and airflow, helping to determine the degree of lung impairment.
- Blood tests: May be used to check for markers of inflammation or specific antibodies related to certain types of pneumonitis, such as those seen in hypersensitivity pneumonitis.
- Bronchoscopy with bronchoalveolar lavage (BAL): A procedure where a thin tube is inserted into the airways to collect fluid samples from the lungs for analysis.
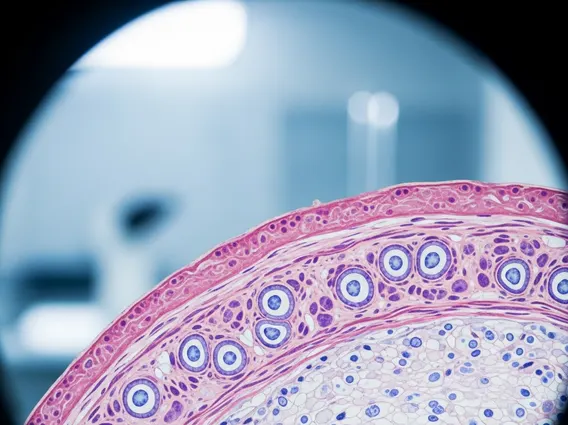
- Lung biopsy: In some cases, a small tissue sample from the lung may be required for microscopic examination to confirm the diagnosis and identify the specific type of inflammation.
Early and accurate diagnosis is crucial for preventing irreversible lung damage, especially in chronic forms of the disease. Treatment focuses on removing the causative agent and may involve corticosteroids to reduce inflammation, along with supportive care to manage symptoms.