Pmn
Pmn, or Polymorphonuclear Leukocyte, plays a crucial role in the body’s defense mechanisms. These specialized white blood cells are frontline responders against infections and inflammation, forming a vital part of the innate immune system.

Key Takeaways
- Polymorphonuclear Leukocytes (PMNs) are a critical type of white blood cell, primarily neutrophils, essential for innate immunity.
- They rapidly respond to sites of infection and inflammation, engulfing and neutralizing pathogens.
- PMN levels are routinely assessed through blood tests, typically as part of a complete blood count (CBC) with differential.
- Abnormal PMN counts can signal various health conditions, including bacterial infections, inflammatory disorders, or bone marrow issues.
- Understanding PMN function and their levels in the blood is fundamental for diagnosing and managing immune-related health concerns.
What is a PMN (Polymorphonuclear Leukocyte)?
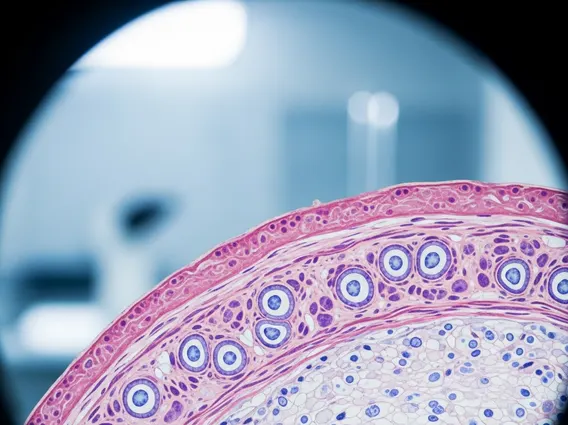
A Polymorphonuclear Leukocyte (PMN) is a type of white blood cell characterized by a multi-lobed nucleus and granular cytoplasm. The PMN medical definition encompasses several cell types, but the term most commonly refers to neutrophils, which constitute the vast majority of PMNs in the human body. These cells are produced in the bone marrow and are crucial components of the innate immune system, providing the body’s first line of defense against invading pathogens.
Neutrophils, specifically, are the most abundant type of granulocyte and represent about 50-70% of all circulating white blood cells in healthy adults. Their distinctive multi-lobed nucleus, which can appear as several distinct segments, gives them their “polymorphonuclear” name. The granules within their cytoplasm contain various enzymes and antimicrobial compounds vital for destroying foreign invaders.
Role of PMNs in the Immune System
The primary PMN function in body is to act as rapid responders to infection and inflammation. Upon detecting signals of infection or tissue damage, PMNs quickly migrate from the bloodstream to the affected site through a process called chemotaxis. Once at the site, they employ several mechanisms to neutralize threats.
- Phagocytosis: PMNs engulf and internalize pathogens, such as bacteria and fungi, into vesicles called phagosomes. These phagosomes then fuse with lysosomes, forming phagolysosomes where the pathogens are destroyed by enzymes and reactive oxygen species.
- Degranulation: PMNs release the contents of their granules, which contain potent antimicrobial proteins and enzymes, directly into the extracellular space to kill pathogens and modulate the immune response.
- Neutrophil Extracellular Traps (NETs): In a process known as NETosis, PMNs can release a web-like structure of decondensed chromatin studded with antimicrobial proteins. These NETs trap and kill pathogens, preventing their spread.
This rapid and potent response makes PMNs indispensable for controlling acute bacterial and fungal infections. For instance, in bacterial infections, PMNs are typically the first immune cells to arrive at the site, often within minutes to hours, playing a critical role in preventing systemic spread. (Source: Medical consensus and various immunology textbooks).
Understanding PMN Levels in Blood Tests
The assessment of PMN levels is a routine part of a complete blood count (CBC) with differential, providing valuable insights into a patient’s immune status. The PMN blood test meaning refers to the count of these specific white blood cells in a blood sample, usually reported as an absolute number or a percentage of total white blood cells.
Variations in PMN counts can indicate underlying health issues. Elevated PMN levels, known as neutrophilia, often suggest an active bacterial infection, inflammation, tissue injury, or physiological stress. Conversely, decreased PMN levels, or neutropenia, can point to conditions like severe infections (e.g., sepsis), bone marrow suppression (due to certain medications, chemotherapy, or autoimmune diseases), or viral infections.
Interpreting PMN levels requires consideration of the patient’s overall clinical picture and other blood test results. Here’s a summary of what different PMN levels might indicate:
| PMN Level | Clinical Term | Potential Implications |
|---|---|---|
| High | Neutrophilia | Bacterial infection, inflammation (e.g., appendicitis, arthritis), trauma, stress, certain cancers (e.g., leukemia), corticosteroid use. |
| Low | Neutropenia | Severe infection (e.g., sepsis), viral infections (e.g., influenza, measles), bone marrow disorders, autoimmune diseases (e.g., lupus), chemotherapy, certain medications. |
| Normal | Normal range | Healthy immune function, no acute infection or severe inflammation detected. |