Endocarditis
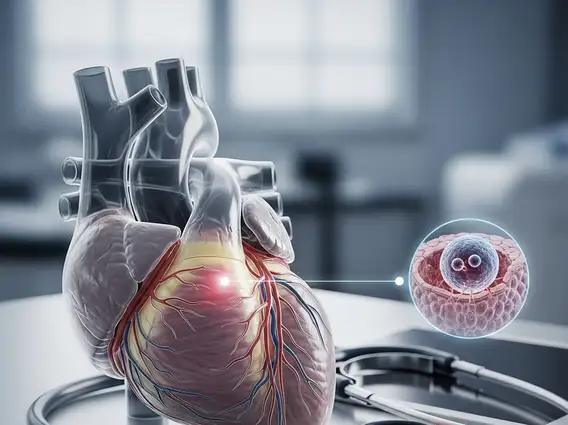
Endocarditis is a serious and potentially life-threatening inflammation of the endocardium, the inner lining of the heart chambers and valves. This condition typically arises when germs, usually bacteria, enter the bloodstream and attach to damaged areas of the heart.
Key Takeaways
- Endocarditis is an inflammation of the heart’s inner lining, often affecting the valves.
- It is primarily caused by bacterial or fungal infections that spread through the bloodstream.
- Symptoms can vary widely but often include fever, fatigue, and new or changing heart murmurs.
- Diagnosis involves blood cultures, echocardiograms, and other imaging tests.
- Treatment typically requires prolonged courses of antibiotics and may necessitate surgical intervention in severe cases.
What is Endocarditis?
Endocarditis is a rare but severe condition characterized by inflammation of the endocardium, the delicate membrane that lines the inside of the heart and its valves. This inflammation is most commonly caused by an infection, usually bacterial, though fungal infections can also be responsible. When pathogens enter the bloodstream, they can settle on damaged heart tissue, particularly the valves, forming vegetations—clumps of bacteria, blood cells, and fibrin. These vegetations can damage the heart valves, disrupt normal blood flow, and potentially lead to serious complications such as heart failure, stroke, or organ damage.
The incidence of infective endocarditis varies globally, but it is estimated to affect approximately 1.7 to 6.2 people per 100,000 annually in developed countries, according to data from the American Heart Association. While it can affect anyone, individuals with pre-existing heart conditions, prosthetic heart valves, or certain medical devices are at a higher risk.
Endocarditis Symptoms and Causes
The symptoms of Endocarditis can be diverse and may develop slowly over weeks or rapidly within days, depending on the type of infection and the individual’s overall health. Common indicators often mimic other illnesses, making early diagnosis challenging. Recognizing these signs is crucial for timely intervention.
Common symptoms include:
- Fever and chills
- Fatigue and weakness
- Aching joints and muscles
- Night sweats
- Shortness of breath
- A new or changed heart murmur
- Swelling in the feet, legs, or abdomen
- Unexplained weight loss
- Small, painful nodules under the skin of the fingers or toes (Osler’s nodes)
- Painless, flat, red spots on the palms and soles (Janeway lesions)
The primary cause of endocarditis is the entry of bacteria or other microorganisms into the bloodstream, a process known as bacteremia. These pathogens can originate from various sources, including dental procedures, skin infections, intravenous drug use, or medical procedures involving catheters. Once in the bloodstream, they can adhere to damaged heart valves or other heart structures, leading to infection and inflammation.
Endocarditis Diagnosis and Treatment
Diagnosing Endocarditis requires a thorough evaluation, as its symptoms can overlap with many other conditions. Healthcare providers typically employ a combination of tests to confirm the presence of the infection and assess its impact on the heart. Prompt and accurate diagnosis is critical for effective management.
The diagnostic process often includes:
| Diagnostic Method | Purpose |
|---|---|
| Blood Cultures | To identify the specific bacteria or fungi causing the infection. Multiple samples are usually taken. |
| Echocardiogram | An ultrasound of the heart to visualize vegetations on the heart valves, assess heart function, and detect valve damage. |
| Electrocardiogram (ECG) | To check for abnormal heart rhythms or signs of heart damage. |
| Blood Tests | To look for signs of inflammation, anemia, and kidney function abnormalities. |
Endocarditis treatment options primarily involve aggressive antibiotic therapy, often administered intravenously for several weeks. The specific antibiotic regimen depends on the identified pathogen and its susceptibility. In some cases, antifungal medications may be used for fungal endocarditis. Close monitoring for treatment response and potential complications is essential.
Surgical intervention may be necessary if the infection does not respond to medication, if there is significant heart valve damage, or if complications such such as heart failure or recurrent emboli occur. Surgery typically involves repairing or replacing the damaged heart valve(s) and removing infected tissue. While antibiotics are the cornerstone of treatment, supportive care for symptoms and complications is also a vital part of the overall management strategy.