Embolism
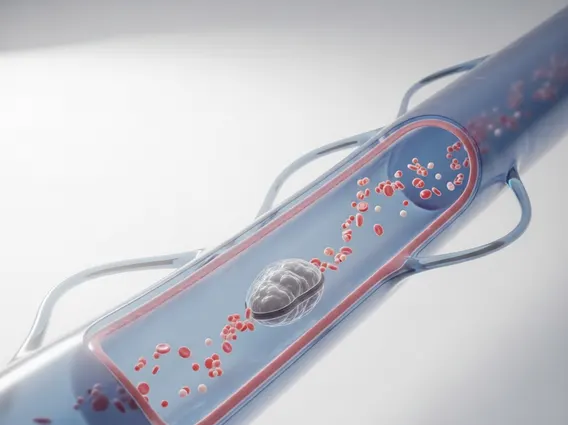
An embolism is a serious medical condition that occurs when an obstruction, such as a blood clot, fat globule, or air bubble, blocks a blood vessel. This blockage can restrict blood flow to vital organs, potentially leading to severe health complications or even death.
Key Takeaways
- An embolism is a blockage in a blood vessel, often caused by a blood clot, fat, or air.
- There are various types, including pulmonary embolism (lungs), arterial embolism (arteries), and venous embolism (veins).
- Symptoms vary depending on the location but can include sudden pain, shortness of breath, and weakness.
- Risk factors include prolonged immobility, surgery, certain medical conditions, and lifestyle choices.
- Prevention often involves managing risk factors, medication, and lifestyle adjustments.
What is an Embolism? Understanding Its Types
An Embolism refers to the sudden blocking of an artery or vein by an embolus, which is any material that travels through the bloodstream and lodges in a vessel too small to pass through. This obstruction can severely impede blood flow, depriving tissues and organs of oxygen and nutrients. Understanding what is an Embolism is crucial for recognizing its potential dangers and seeking timely medical attention.
The nature of the embolus determines the specific type of embolism. While blood clots are the most common cause, other substances can also lead to blockages. According to the Centers for Disease Control and Prevention (CDC), deep vein thrombosis (DVT) and pulmonary embolism (PE) affect an estimated 900,000 people in the United States each year, with PE being a life-threatening form of embolism.
There are several primary types of embolism, categorized by the material causing the blockage or the location of the obstruction:
- Pulmonary Embolism (PE): This occurs when a blood clot (usually from a deep vein in the leg) travels to the lungs, blocking one or more pulmonary arteries. It can cause sudden shortness of breath, chest pain, and rapid heart rate.
- Arterial Embolism: Typically originating from the heart, these clots travel through arteries and can block blood flow to organs like the brain (leading to stroke), limbs, or kidneys.
- Venous Embolism: While often associated with PE, venous embolisms can also occur in other veins, though they are less common than arterial blockages causing acute organ damage.
- Fat Embolism: This type involves fat globules entering the bloodstream, often after a major trauma like a bone fracture or surgery. They can travel to the lungs or brain.
- Air Embolism: Caused by air bubbles entering a vein or artery, typically during surgery, diving accidents, or certain medical procedures.
- Amniotic Fluid Embolism: A rare but severe complication during pregnancy or childbirth, where amniotic fluid enters the mother’s bloodstream.
Embolism Symptoms, Causes, and Risk Factors
Recognizing Embolism symptoms and causes is vital for early diagnosis and treatment. Symptoms vary widely depending on the type and location of the embolism, but they often appear suddenly and can be severe. For instance, a pulmonary embolism might cause sudden shortness of breath, chest pain that worsens with deep breaths, coughing (sometimes with blood), and rapid heart rate. An arterial embolism in a limb could lead to sudden, severe pain, numbness, coolness, and paleness in the affected area.
The underlying causes of an embolism are diverse. Blood clot embolisms, the most common type, often form due to conditions that affect blood flow, blood vessel walls, or blood clotting mechanisms. Other causes include trauma, surgery, and certain medical procedures. Risk factors significantly increase an individual’s likelihood of developing an embolism. These include:
- Prolonged Immobility: Long flights, bed rest, or paralysis can slow blood flow, promoting clot formation.
- Surgery or Trauma: Especially orthopedic surgeries (hip or knee replacement) and major injuries, which can release fat globules or trigger clotting.
- Certain Medical Conditions: Heart conditions (e.g., atrial fibrillation), cancer, inflammatory bowel disease, and inherited clotting disorders.
- Lifestyle Factors: Smoking, obesity, and a sedentary lifestyle contribute to poor vascular health.
- Hormonal Factors: Use of estrogen-containing birth control pills or hormone replacement therapy, and pregnancy.
Understanding these factors allows healthcare providers to assess individual risk and implement preventive measures.
Preventing and Managing Embolism
Effective strategies for How to prevent an embolism focus on minimizing risk factors and, when necessary, using medical interventions. Prevention is particularly important for individuals at high risk due to surgery, chronic conditions, or lifestyle. Management involves immediate medical treatment to dissolve or remove the embolus and prevent recurrence.
Preventive measures often include:
- Anticoagulant Medications: Blood thinners are frequently prescribed for individuals at high risk of clot formation, such as after surgery or for those with atrial fibrillation.
- Compression Stockings: These can help improve blood flow in the legs and prevent deep vein thrombosis (DVT).
- Early Mobilization: After surgery or during periods of bed rest, moving as soon as medically appropriate can significantly reduce the risk of clots.
- Lifestyle Modifications: Regular exercise, maintaining a healthy weight, quitting smoking, and staying hydrated are crucial for overall vascular health.
- Intermittent Pneumatic Compression Devices: These devices are used in hospitals to apply pressure to the legs, promoting blood circulation.
Management of an acute embolism typically involves emergency medical care. This may include thrombolytic drugs to dissolve clots, surgical removal of the embolus (embolectomy), or placement of a vena cava filter to prevent clots from reaching the lungs. Long-term management often includes continued anticoagulant therapy and addressing underlying conditions to prevent future episodes.
