Conventional Mammography
Conventional mammography is a vital imaging technique used for breast cancer screening and diagnosis. It plays a crucial role in the early detection of abnormalities, which can significantly improve treatment outcomes.
Key Takeaways
- Conventional mammography is an X-ray imaging method for the breasts, primarily used for early breast cancer detection.
- The procedure involves compressing the breast to spread tissue evenly, allowing for clearer X-ray images.
- It works by using low-dose X-rays to create detailed images, which radiologists then examine for signs of cancer.
- Key benefits include reduced breast cancer mortality rates due to early detection and its proven effectiveness as a screening tool.
- Regular screening with mammography is recommended for many women, especially those over 40, to catch potential issues early.
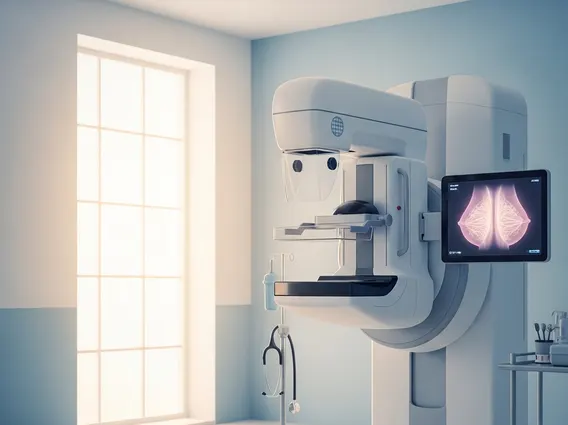
What is Conventional Mammography?
What is conventional mammography? It is a specialized medical imaging technique that uses a low-dose X-ray system to examine breasts. Often referred to simply as a mammogram, its primary purpose is to detect breast cancer early, sometimes years before a lump can be felt by physical examination. This imaging method is fundamental in both screening for breast cancer in asymptomatic women and diagnosing breast conditions in women experiencing symptoms like a lump, pain, or nipple discharge. By creating detailed images of the internal breast tissue, radiologists can identify subtle changes that may indicate the presence of cancer or other benign conditions.
The procedure is a cornerstone of breast health, allowing for timely intervention and improved prognoses. It helps differentiate between various types of breast tissue and identify calcifications or masses that might be cancerous. Understanding what is conventional mammography is key to appreciating its role in public health initiatives aimed at reducing breast cancer mortality.
How Conventional Mammography Works
The process of conventional mammography procedure involves several steps designed to obtain clear and accurate images of the breast tissue. During the examination, a specially trained technologist will position each breast individually on a platform. The breast is then gently but firmly compressed between two plates. This compression is essential for several reasons: it flattens the breast to spread the tissue evenly, reducing the thickness of the breast so that a lower X-ray dose can be used, minimizing radiation exposure, and holding the breast still to prevent blurring of the image caused by movement. It also helps to visualize all the breast tissue and reduce overlapping shadows.
Once the breast is positioned and compressed, a low-dose X-ray beam passes through the tissue, creating an image on a detector. Typically, two views are taken of each breast: one from top to bottom (cranial-caudal view) and one from side to side at an angle (mediolateral oblique view). These images, called mammograms, are then reviewed by a radiologist who specializes in breast imaging. The radiologist looks for any abnormalities, such as masses, distortions, or microcalcifications, which could be signs of cancer. This detailed process explains how conventional mammography works to provide critical diagnostic information.
Key Benefits of Conventional Mammography
The benefits of conventional mammography are significant, primarily centered around its ability to detect breast cancer at an early stage, often before it can be felt. Early detection is crucial because it allows for more effective treatment options and significantly improves survival rates. According to the Centers for Disease Control and Prevention (CDC), regular mammograms can help find breast cancer early when it is small and easier to treat, leading to better outcomes for women. This early identification can mean the difference between localized treatment and more extensive interventions, such as chemotherapy or radiation.
Furthermore, conventional mammography is a widely available and well-established screening tool with decades of proven effectiveness. Its widespread use has contributed to a notable decline in breast cancer mortality rates in many countries. For example, the American Cancer Society indicates that the breast cancer death rate declined by 43% from 1989 to 2020 among women, partly attributed to advances in early detection, including mammography. The procedure is also relatively quick and non-invasive, making it a practical option for routine screening. These compelling advantages underscore why conventional mammography remains a cornerstone of breast health management and a critical tool in the fight against breast cancer.
