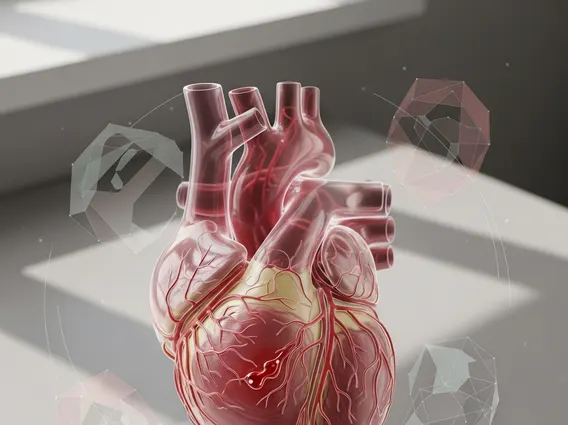
Blood Stasis
Blood stasis refers to a condition where blood flow is impaired or stagnant within the body’s vessels. This can lead to a range of symptoms and potentially impact overall health by hindering the delivery of oxygen and nutrients to tissues.
Key Takeaways
- Blood stasis involves impaired or stagnant blood circulation, affecting various body parts.
- Symptoms often include localized pain, dark complexion, and specific menstrual irregularities.
- Causes can range from physical trauma and inflammation to lifestyle factors and underlying health conditions.
- Diagnosis typically involves a thorough medical history, physical examination, and sometimes imaging.
- Treatment focuses on improving circulation through lifestyle changes, medication, and sometimes complementary therapies.
What is Blood Stasis?
What is blood stasis? It is a medical term describing a state where blood circulation is compromised, leading to a pooling or sluggish movement of blood in certain areas of the body. This phenomenon can occur in various parts of the circulatory system, including veins, arteries, and capillaries. When blood fails to flow smoothly, it can accumulate, leading to localized congestion and a lack of proper perfusion to tissues and organs. This impaired circulation can prevent cells from receiving adequate oxygen and nutrients, while also hindering the removal of waste products.
Understanding what is Blood Stasis is crucial because it is not merely a symptom but can be an underlying factor in numerous health issues. The condition is characterized by a deviation from normal, free-flowing blood dynamics, often resulting in observable physical signs and internal discomfort. While sometimes associated with specific medical conditions like deep vein thrombosis, the broader concept of blood stasis encompasses any form of circulatory impediment that leads to localized congestion or reduced blood flow.
Symptoms and Causes of Blood Stasis
Recognizing the signs and understanding the origins of impaired circulation are vital steps in addressing this condition. The presentation of blood stasis symptoms causes can vary widely depending on the affected area and the severity of the stagnation.
Common Symptoms of Blood Stasis
The presence of blood stasis symptoms often manifests as specific types of pain and observable physical changes. Pain associated with blood stasis is typically described as sharp, fixed, and localized, often worsening at night or with pressure. Unlike migratory pain, stasis-related pain tends to remain in one specific area. Other common indicators include a dark or dusky complexion, particularly in the affected region, and a purplish discoloration of the tongue or lips. Women may experience severe menstrual pain with dark, clotted blood, or irregular menstrual cycles. Additionally, palpable masses or lumps that are tender to the touch can sometimes indicate underlying blood stagnation.
- Localized Pain: Sharp, stabbing, or fixed pain that does not easily move.
- Dark Complexion: Dusky skin tone, especially in areas with poor circulation.
- Purple Tongue/Lips: A noticeable purplish hue, indicating poor oxygenation.
- Menstrual Irregularities: Painful periods with dark, clotted blood.
- Palpable Masses: Tender lumps or nodules under the skin.
Underlying Causes of Blood Stasis
The blood stasis causes are diverse and can stem from a combination of factors. Physical trauma, such as injuries or surgery, can directly damage blood vessels and impede flow. Chronic inflammation within the body can also contribute by altering vessel integrity and promoting sluggish circulation. Lifestyle factors play a significant role; prolonged periods of immobility, a sedentary lifestyle, and poor dietary choices lacking essential nutrients can all contribute to the development of blood stasis. Furthermore, certain medical conditions like varicose veins, atherosclerosis, or disorders affecting blood clotting mechanisms can predispose individuals to this circulatory issue. For example, conditions that increase blood viscosity or damage vessel walls can significantly increase the risk of developing blood stasis.
Diagnosing and Treating Blood Stasis
Effectively managing blood stasis requires accurate diagnosis and a tailored treatment plan. A healthcare professional will consider various factors to determine the presence and extent of the condition.
How to Diagnose Blood Stasis
How to diagnose blood stasis typically begins with a comprehensive medical history and a thorough physical examination. The physician will inquire about the nature of symptoms, their duration, and any aggravating or alleviating factors. During the physical exam, the doctor will look for visible signs such as skin discoloration, palpable masses, and assess the quality of pulses. In some cases, diagnostic imaging techniques like Doppler ultrasound may be used to visualize blood flow and identify blockages or areas of stagnation within vessels. Blood tests might also be conducted to check for underlying conditions that could contribute to stasis, such as clotting disorders or inflammatory markers. It is essential to consult a healthcare provider for an accurate diagnosis, as self-diagnosis can be misleading.
Blood Stasis Treatment Options
The array of blood stasis treatment options aims to improve circulation, alleviate symptoms, and address underlying causes. Treatment often involves a multi-faceted approach. Lifestyle modifications are frequently recommended, including regular physical activity to promote blood flow, dietary changes to support vascular health (e.g., reducing saturated fats, increasing fiber), and adequate hydration. Medications may be prescribed to thin the blood, reduce inflammation, or improve vessel tone, depending on the specific cause of the stasis. In some instances, physical therapy or specialized exercises might be beneficial. While complementary therapies such as acupuncture or certain herbal remedies are sometimes explored, it is crucial to understand that these should be used as supportive measures and do not replace conventional medical treatment. Always discuss any complementary therapies with your doctor to ensure they are safe and appropriate for your condition.
Disclaimer: The information provided in this article is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
