Urethral Cancer Stages
Understanding urethral cancer stages is crucial for effective diagnosis, treatment planning, and predicting patient outcomes. This article provides a comprehensive overview of how urethral cancer is staged, the characteristics of each stage, associated symptoms, and the implications for prognosis and treatment.
Key Takeaways
- Accurate staging of urethral cancer is vital for determining the most appropriate treatment strategy and predicting patient prognosis.
- The TNM (Tumor, Node, Metastasis) system is the primary method used to classify urethral cancer stages, detailing tumor size, lymph node involvement, and distant spread.
- Urethral cancer progresses from early stages (0 and I), which are localized, to advanced stages (II, III, and IV), indicating deeper invasion or metastasis.
- Symptoms can vary significantly by stage, with early indicators often including urinary changes, while advanced stages may present with more systemic or severe localized issues.
- Treatment options and urethral cancer prognosis by stage differ substantially, with early stages generally having better outcomes and more localized treatments.
Understanding Urethral Cancer Staging
Staging is a critical process in oncology that determines the extent of cancer within the body. For urethral cancer, this process helps medical professionals understand how far the cancer has spread from its origin in the urethra. Accurate staging is paramount for guiding treatment decisions and providing patients with an informed outlook on their condition.
Importance of Accurate Staging
The importance of accurate urethral cancer staging explained lies in its direct impact on patient management. It allows oncologists to select the most effective therapies, whether surgical, radiation-based, or systemic. For instance, localized cancers may be treated with surgery alone, while more advanced stages might require a combination of therapies. Moreover, staging provides a basis for predicting the likely course of the disease and the patient’s survival rate, which is essential for both medical planning and patient counseling. According to the National Cancer Institute (NCI), precise staging is a cornerstone of personalized cancer care, ensuring treatments are tailored to the specific characteristics of the tumor.
Overview of Staging Systems
The most widely accepted system for understanding urethral cancer stages is the TNM classification system, developed by the American Joint Committee on Cancer (AJCC) and the Union for International Cancer Control (UICC). This system evaluates three key aspects of the cancer: the primary Tumor (T), involvement of regional lymph Nodes (N), and presence of distant Metastasis (M). Each of these components is assigned a numerical value or letter, which are then combined to determine the overall stage of the cancer, ranging from Stage 0 to Stage IV.
How Urethral Cancer Stages Are Determined
Determining the stage of urethral cancer involves a series of diagnostic tests and a thorough evaluation by a multidisciplinary team of specialists. This comprehensive approach ensures that all relevant information is gathered to accurately classify the cancer’s extent.
Diagnostic Tests for Staging
To determine how is urethral cancer staged, doctors employ various diagnostic procedures. These tests help visualize the tumor, assess its depth of invasion, and check for spread to lymph nodes or distant organs:
- Cystoscopy and Biopsy: A thin, lighted tube (cystoscope) is inserted into the urethra to visualize the lining. Suspicious areas are biopsied for pathological examination to confirm cancer and determine its type.
- Imaging Tests:
- CT Scan (Computed Tomography): Provides detailed cross-sectional images of the abdomen and pelvis to check for tumor spread to lymph nodes or other organs.
- MRI (Magnetic Resonance Imaging): Offers high-resolution images, particularly useful for assessing the depth of tumor invasion into the urethral wall and surrounding tissues.
- PET Scan (Positron Emission Tomography): Often combined with CT (PET-CT), it can detect metabolically active cancer cells throughout the body, identifying distant metastases.
- Physical Examination: A thorough physical exam, including a pelvic exam for women and a digital rectal exam for men, can help detect palpable masses or enlarged lymph nodes.
TNM Classification System Explained
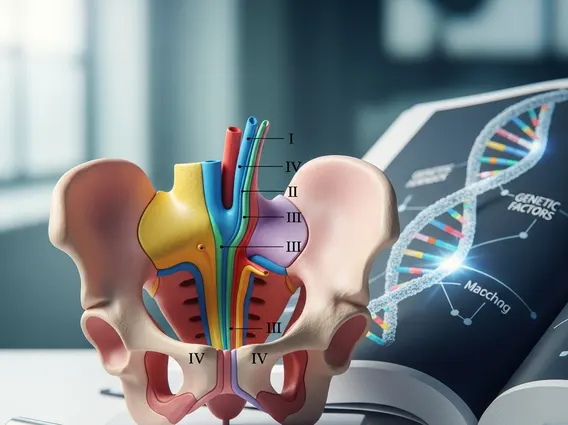
The TNM system is a standardized method for describing the anatomical extent of cancer. Each letter represents a different aspect:
- T (Tumor): Describes the size and extent of the primary tumor.
- Ta: Non-invasive papillary carcinoma.
- Tis: Carcinoma in situ (flat tumor, not invading tissue).
- T1: Tumor invades subepithelial connective tissue.
- T2: Tumor invades the urethral muscularis (muscle layer).
- T3: Tumor invades adjacent organs (e.g., prostate, vagina, bladder neck).
- T4: Tumor invades other adjacent organs or structures (e.g., rectum, pelvic wall).
- N (Nodes): Indicates whether the cancer has spread to regional lymph nodes.
- N0: No regional lymph node metastasis.
- N1: Metastasis in a single regional lymph node.
- N2: Metastasis in multiple regional lymph nodes or a single node with extracapsular extension.
- M (Metastasis): Denotes whether the cancer has spread to distant parts of the body.
- M0: No distant metastasis.
- M1: Distant metastasis present.
These T, N, and M categories are then combined to assign an overall stage, providing a comprehensive picture of the cancer’s progression.
Detailed Urethral Cancer Stages (0-IV)
The classification of urethral cancer stage 1 2 3 4, along with Stage 0, provides a clear framework for understanding the disease’s progression. Each stage represents a distinct level of tumor invasion and spread, influencing treatment choices and prognosis.
Early Stages: 0 and I Characteristics
- Stage 0 (Carcinoma in Situ – Tis): This is the earliest form of urethral cancer. The cancer cells are found only in the innermost lining of the urethra and have not invaded the deeper tissues. It is considered non-invasive.
- Stage I (T1, N0, M0): In Stage I, the tumor has grown into the subepithelial connective tissue, which is just beneath the lining of the urethra. However, it has not spread to the muscle layer, regional lymph nodes, or distant sites. This stage is still considered localized and highly treatable.
Advanced Stages: II, III, and IV
- Stage II (T2, N0, M0): At Stage II, the cancer has invaded the muscular layer of the urethra (muscularis). It has not spread to regional lymph nodes or distant organs. The deeper invasion signifies a more advanced local disease compared to Stage I.
- Stage III (T3, N0/N1, M0 or T4, N0, M0): Stage III indicates that the tumor has grown beyond the urethral wall to invade adjacent organs or structures. This could include the prostate, vagina, or bladder neck. It may or may not involve regional lymph nodes (N0 or N1), but there is no distant metastasis.
- Stage IV (Any T, N2, M0 or Any T, Any N, M1): This is the most advanced stage of urethral cancer. It is characterized by either extensive involvement of regional lymph nodes (N2) or the presence of distant metastasis (M1), meaning the cancer has spread to organs far from the urethra, such as the lungs, liver, or bones. Stage IV cancer requires aggressive, systemic treatment approaches.
Symptoms Associated with Each Stage
The stages of urethral cancer symptoms can vary significantly depending on how far the cancer has progressed. Recognizing these symptoms early can lead to a quicker diagnosis and potentially more effective treatment.
Early Stage Indicators
In the early stages (0 and I), symptoms are often subtle and can mimic those of less serious urinary tract conditions. Common early stages of urethral cancer symptoms include:
- Hematuria: Blood in the urine, which may be visible (gross hematuria) or only detectable under a microscope (microscopic hematuria). This is often one of the first and most common signs.
- Dysuria: Pain or burning sensation during urination.
- Frequent Urination: An increased urge to urinate, often without a significant increase in urine volume.
- Weak or Interrupted Urine Stream: Difficulty maintaining a steady flow of urine.
- Palpable Mass: In some cases, a lump or mass may be felt along the urethra, particularly in women.
Advanced Stage Manifestations
As urethral cancer progresses to Stages II, III, and IV, the symptoms become more pronounced and may indicate local invasion or distant spread. Advanced stage manifestations can include:
- Urinary Incontinence: Loss of bladder control, ranging from mild leakage to complete inability to hold urine.
- Pelvic Pain: Persistent pain in the pelvic area, lower abdomen, or perineum, indicating tumor invasion into surrounding tissues or organs.
- Swelling in Legs: If the cancer has spread to lymph nodes in the groin or pelvis, it can obstruct lymphatic drainage, leading to swelling (lymphedema) in the legs.
- Weight Loss and Fatigue: Unexplained weight loss, loss of appetite, and persistent fatigue are systemic symptoms often associated with advanced cancer.
- Bone Pain: If the cancer has metastasized to the bones, it can cause localized bone pain.
- Fistula Formation: In very advanced cases, the tumor may erode through tissues, creating an abnormal connection (fistula) between the urethra and other organs like the vagina or rectum, leading to leakage of urine or stool.
Prognosis and Treatment Options by Stage
The urethral cancer prognosis by stage varies significantly, with early detection and localized disease generally leading to better outcomes. Treatment strategies are carefully tailored to the specific stage and characteristics of the cancer, as well as the patient’s overall health.
Treatment Strategies for Early Stages
For early urethral cancer stages (0 and I), the primary goal is to remove the cancer while preserving as much of the urethra and its function as possible. The urethral cancer prognosis by stage is generally favorable at these stages.
- Transurethral Resection of Bladder Tumor (TURBT) or Endoscopic Resection: For Stage 0 (Tis) and some superficial Stage I tumors, cancer can often be removed endoscopically through the urethra.
- Partial Urethrectomy: If the tumor is small and localized, a portion of the urethra containing the cancer may be surgically removed. The remaining ends are then reconnected.
- Laser Ablation: In some cases, a laser can be used to destroy cancer cells.
- Intracavitary Chemotherapy or Immunotherapy: Medications may be instilled directly into the urethra or bladder to target remaining cancer cells, particularly for carcinoma in situ.
According to the American Cancer Society, localized urethral cancer has a significantly higher 5-year survival rate compared to regional or distant disease, underscoring the importance of early diagnosis and treatment.
Managing Advanced Urethral Cancer
Treatment for advanced urethral cancer stages (II, III, and IV) is more complex and often involves a combination of therapies aimed at eradicating the cancer, controlling its spread, and managing symptoms. The urethral cancer prognosis by stage becomes less favorable as the disease advances, necessitating more aggressive approaches.
- Radical Urethrectomy: This involves the complete surgical removal of the urethra and surrounding structures. In men, this may include the penis, prostate, and lymph nodes. In women, it may involve the urethra, bladder, and part of the vagina. Urinary diversion surgery (creating a new way for urine to leave the body) is typically performed afterward.
- Radiation Therapy: High-energy rays are used to kill cancer cells. It can be used as a primary treatment, after surgery to eliminate any remaining cancer cells (adjuvant therapy), or to relieve symptoms (palliative therapy).
- Chemotherapy: Anti-cancer drugs are administered intravenously or orally to kill cancer cells throughout the body. It is often used for advanced or metastatic disease, sometimes before surgery (neoadjuvant) to shrink tumors or after surgery (adjuvant) to prevent recurrence.
- Immunotherapy: These treatments harness the body’s immune system to fight cancer. Drugs like checkpoint inhibitors can be used for advanced urethral cancer, especially if it has spread or recurred after other treatments.
- Targeted Therapy: These drugs specifically target certain molecules involved in cancer growth and spread, often with fewer side effects than traditional chemotherapy.
Treatment plans for advanced stages are highly individualized and often involve a multidisciplinary team to optimize outcomes and quality of life.
Frequently Asked Questions
What is the most common type of urethral cancer?
The most common type of urethral cancer varies by location within the urethra. Transitional cell carcinoma (TCC) is prevalent in the part of the urethra closest to the bladder, similar to bladder cancer. Squamous cell carcinoma (SCC) is more common in the distal urethra and in men, particularly in the penile urethra. Adenocarcinoma, which originates from glandular cells, is less common but can occur anywhere along the urethra, often associated with urethral diverticula.
How often should follow-up appointments be after treatment for urethral cancer?
After treatment for urethral cancer, regular follow-up appointments are crucial for monitoring recurrence and managing potential side effects. The frequency typically depends on the initial stage of the cancer and the type of treatment received. Initially, appointments may be every 3-6 months for the first few years, gradually extending to annually. These visits often include physical exams, cystoscopies, and imaging tests to ensure early detection of any new or returning cancer.
Is urethral cancer more common in men or women?
Urethral cancer is generally considered rare, but its incidence differs between sexes. It is slightly more common in women, though when it occurs in men, it tends to be more aggressive and often diagnosed at a later stage. The anatomical differences in the male and female urethra, as well as varying risk factors such as chronic inflammation or sexually transmitted infections, contribute to these differences in prevalence and disease presentation.
