Survival Rate and Prognosis for Melanoma
Understanding the potential outcomes and influencing factors is crucial for individuals diagnosed with melanoma, a serious form of skin cancer. This article delves into the statistics and elements that shape an individual’s outlook, providing clarity on the journey ahead.
Key Takeaways
- Melanoma survival rate is significantly influenced by the stage at diagnosis, with early detection leading to much better outcomes.
- Various factors, including tumor characteristics and patient health, play a critical role in determining an individual’s melanoma prognosis.
- Advances in treatment, particularly immunotherapy and targeted therapies, have substantially improved the melanoma treatment and survival outlook for many patients.
- Regular follow-up and self-monitoring are essential for detecting recurrence and ensuring long-term survival with melanoma.
- While statistics provide a general overview, each patient’s journey is unique, emphasizing the importance of personalized medical advice.
Melanoma Survival Rates by Stage
The melanoma survival rate is a critical piece of information for patients and clinicians, offering insight into the typical course of the disease. These rates are usually presented as 5-year or 10-year survival statistics, indicating the percentage of people who are still alive five or ten years after diagnosis. It’s important to remember that these are averages and individual experiences can vary widely. The most significant determinant of these rates is the stage at which the melanoma is diagnosed.
According to leading health organizations like the American Cancer Society and the National Cancer Institute, melanoma survival rates by stage show a clear trend: the earlier the diagnosis, the higher the survival rate. This underscores the importance of regular skin checks and prompt medical evaluation of suspicious moles.
Early-Stage Melanoma Outlook
For individuals diagnosed with early-stage melanoma, the outlook is generally very positive. This includes melanoma in situ (Stage 0) and localized melanoma (Stages I and II), where the cancer has not spread beyond the original tumor site. For localized melanoma, the 5-year survival rate is exceptionally high, often exceeding 90-95%. This favorable melanoma life expectancy statistics for early stages is largely due to the effectiveness of surgical removal when the tumor is confined.
Even for thicker localized melanomas (Stage II), where the risk of recurrence is slightly higher, the 5-year survival rates remain strong, typically in the range of 70-85%. Early detection allows for complete surgical excision, which is often curative.
Advanced Melanoma Statistics
When melanoma has spread, the melanoma life expectancy statistics become more challenging, but significant advancements in treatment have dramatically improved outcomes in recent years. For regional melanoma (Stage III), where the cancer has spread to nearby lymph nodes but not distant organs, the 5-year survival rates can range from approximately 30% to 70%, depending on the extent of lymph node involvement and other factors. This variability highlights the complexity of understanding melanoma prognosis in advanced stages.
For distant melanoma (Stage IV), where the cancer has spread to distant organs, the 5-year survival rate has historically been lower, often in the range of 15-25%. However, with the advent of new immunotherapies and targeted therapies, many patients with advanced melanoma are now experiencing longer survival times and improved quality of life. These statistics are continually being updated as new treatments become more widespread and effective.
Factors Affecting Melanoma Prognosis
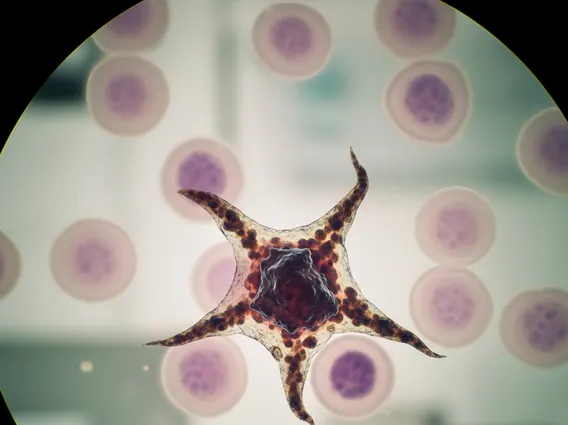
Beyond the stage of cancer, several other factors affecting melanoma survival play a crucial role in determining what is the prognosis for melanoma for an individual patient. These factors can be broadly categorized into characteristics of the tumor itself and patient-specific attributes. A comprehensive evaluation of these elements helps oncologists provide a more personalized prognosis.
Tumor Characteristics
- Breslow Thickness: This is the most important prognostic factor for localized melanoma, measuring how deep the melanoma has grown into the skin. Thinner melanomas (less than 1 mm) have a better prognosis.
- Ulceration: The presence of ulceration (a break in the skin surface over the tumor) indicates a more aggressive tumor and is associated with a poorer prognosis.
- Mitotic Rate: This refers to how quickly the cancer cells are dividing. A higher mitotic rate suggests faster growth and a less favorable outlook.
- Lymph Node Involvement: If melanoma cells are found in nearby lymph nodes, it indicates the cancer has started to spread, significantly impacting the prognosis.
- Distant Metastasis: The presence and location of spread to distant organs (e.g., lungs, brain, liver) are critical in determining the prognosis for Stage IV melanoma.
Patient-Specific Factors
- Age: Younger patients generally tend to have a better prognosis than older patients, though this can vary.
- General Health and Immune Status: A strong immune system and good overall health can help patients tolerate treatment better and potentially fight the cancer more effectively.
- Tumor Location: Melanomas on certain body sites, such as the scalp, neck, hands, or feet, can sometimes be associated with a slightly less favorable prognosis, possibly due to delayed detection or lymphatic drainage patterns.
- Gender: Some studies suggest a slight difference in survival rates between men and women, with women sometimes having a marginally better prognosis.
Treatment’s Impact on Melanoma Survival
The landscape of melanoma treatment and survival outlook has undergone a revolutionary transformation in recent years. Modern therapeutic approaches have significantly improved the prospects for many patients, even those with advanced disease. The choice of treatment is highly individualized, based on the melanoma stage, genetic mutations within the tumor, and the patient’s overall health.
Current Treatment Approaches
Surgery remains the primary treatment for early-stage melanoma, often leading to a complete cure. For more advanced stages, a combination of therapies is typically employed:
- Immunotherapy: These treatments, such as checkpoint inhibitors (e.g., pembrolizumab, nivolumab), harness the body’s own immune system to recognize and destroy cancer cells. They have shown remarkable success in improving long-term survival with melanoma for many patients with advanced disease.
- Targeted Therapy: For melanomas with specific genetic mutations (e.g., BRAF mutations), targeted drugs (e.g., dabrafenib, vemurafenib) can specifically block the growth pathways of cancer cells, leading to significant tumor shrinkage and improved survival.
- Radiation Therapy: While not a primary treatment for melanoma, radiation can be used to control symptoms, treat melanoma that has spread to specific areas (like the brain or bones), or as adjuvant therapy after surgery in some high-risk cases.
- Chemotherapy: Historically used for advanced melanoma, chemotherapy is now less common due to the superior efficacy and fewer side effects of immunotherapy and targeted therapies, but it may still be an option in specific situations.
These advanced treatments have profoundly altered what is the prognosis for melanoma, offering hope where little existed before.
Post-Treatment Monitoring
After initial treatment, ongoing surveillance is a critical component of understanding melanoma prognosis and ensuring the best possible long-term outcomes. Regular follow-up appointments with dermatologists and oncologists are essential. These appointments typically involve comprehensive skin exams to check for new melanomas or signs of recurrence, as well as lymph node examinations. Imaging tests (such as CT scans, PET scans, or MRI) may be performed periodically, especially for patients with a history of advanced melanoma, to detect any internal spread or recurrence.
Patients are also educated on self-skin exams and the importance of reporting any new or changing moles promptly. This vigilant monitoring helps to catch any recurrence at its earliest, most treatable stage, significantly contributing to long-term survival with melanoma.
Long-Term Outlook for Melanoma Patients
Achieving long-term survival with melanoma is increasingly common, particularly with early detection and the advancements in treatment. However, the journey doesn’t end with the completion of initial therapy. Patients must remain vigilant and proactive in managing their health to maintain a positive outlook.
Recurrence Risk
Despite successful initial treatment, there is always a risk of melanoma recurrence. This risk varies significantly based on the initial stage of the cancer and other prognostic factors. Recurrence can manifest in several ways:
- Local Recurrence: The melanoma reappears at or very near the original tumor site.
- Regional Recurrence: The cancer returns in nearby lymph nodes or skin areas (in-transit metastases).
- Distant Recurrence: The melanoma spreads to distant organs, indicating a more advanced stage.
The highest risk of recurrence is typically within the first few years after diagnosis, which is why intensive monitoring is crucial during this period. Patients with thicker melanomas, ulcerated tumors, or lymph node involvement have a higher risk of recurrence, necessitating more frequent and thorough follow-up.
Living Beyond Melanoma
For many, living beyond melanoma involves a commitment to ongoing health management and lifestyle adjustments. This includes strict sun protection practices, such as wearing protective clothing, seeking shade, and using broad-spectrum sunscreen daily, to reduce the risk of developing new melanomas. Regular self-skin exams are also vital for early detection.
Beyond physical health, addressing the psychological and emotional impact of a melanoma diagnosis is important. Support groups, counseling, and open communication with healthcare providers can help patients cope with anxiety about recurrence and adjust to life after cancer. Understanding melanoma prognosis involves not just statistics but also embracing a proactive approach to well-being and maintaining a strong partnership with one’s medical team.
Frequently Asked Questions
How is melanoma survival rate calculated?
Melanoma survival rates are typically calculated based on 5-year or 10-year periods, representing the percentage of patients who are still alive five or ten years after their initial diagnosis. These statistics are derived from large population studies and cancer registries, such as those maintained by the National Cancer Institute. They are often broken down by cancer stage at diagnosis, providing a general benchmark for patient outcomes. It’s crucial to understand these are averages, and individual prognoses can vary based on specific circumstances.
What are the most significant factors influencing melanoma prognosis?
The most significant factor influencing melanoma prognosis is the stage of the cancer at diagnosis, particularly the Breslow thickness (tumor depth) and whether it has spread to lymph nodes or distant organs. Other crucial factors include the presence of ulceration on the tumor, the mitotic rate (how fast cells are dividing), and specific genetic mutations within the tumor. Patient-specific factors like age, overall health, and the tumor’s location can also play a role in the overall outlook.
Can melanoma be cured?
Yes, melanoma can often be cured, especially when detected and treated at an early stage. For localized melanoma (Stage 0, I, or II), surgical removal is frequently curative, leading to very high 5-year survival rates. Even for some advanced melanomas, significant advancements in treatments like immunotherapy and targeted therapy have led to long-term remission and improved survival for many patients, though a complete “cure” for advanced stages is still more challenging to achieve.
