Supracervical Hysterectomy
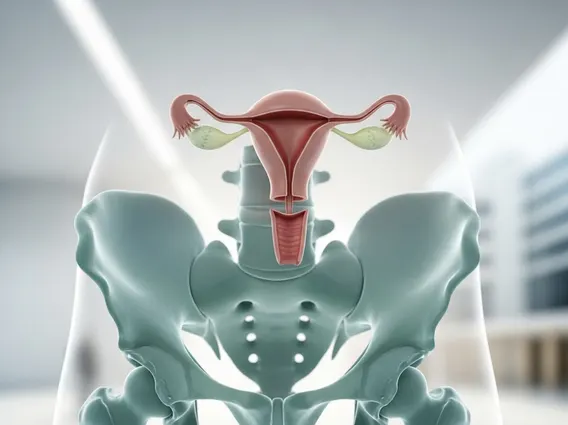
Supracervical Hysterectomy is a surgical procedure involving the removal of the uterus while preserving the cervix. This approach is often considered for individuals seeking relief from various gynecological conditions while aiming to maintain certain aspects of pelvic anatomy.
Key Takeaways
- Supracervical Hysterectomy involves removing the uterus but leaving the cervix intact.
- The procedure can be performed through various methods, including laparoscopic, robotic, or open surgery.
- Potential benefits include a shorter recovery time and reduced risk of certain complications compared to total hysterectomy.
- Unlike total hysterectomy, the cervix remains, necessitating continued cervical cancer screening (Pap tests).
- The choice between supracervical and total hysterectomy depends on individual medical conditions and patient preferences.
What is Supracervical Hysterectomy?
Supracervical Hysterectomy is a surgical procedure in which the main body of the uterus (fundus and corpus) is removed, but the cervix is intentionally left in place. This differs from a total hysterectomy, where the entire uterus, including the cervix, is removed. The procedure is typically performed to address conditions such as uterine fibroids, abnormal uterine bleeding, or adenomyosis, when conservative treatments have not been effective. By preserving the cervix, some patients may experience benefits related to pelvic support and sexual function.
The decision to undergo a Supracervical Hysterectomy is made after careful consideration of a patient’s medical history, symptoms, and future reproductive desires. It is a significant surgical intervention aimed at improving quality of life for individuals suffering from chronic and debilitating uterine conditions.
Supracervical Hysterectomy Procedure Details and Benefits
The supracervical hysterectomy procedure details vary depending on the surgical approach chosen. It can be performed through several methods:
- Laparoscopic Supracervical Hysterectomy (LSH): This minimally invasive approach involves small incisions in the abdomen, through which a laparoscope (a thin, lighted tube with a camera) and surgical instruments are inserted. The uterus is then detached from its supporting structures and removed in pieces through one of the small incisions.
- Robotic-Assisted Supracervical Hysterectomy: Similar to LSH, this method utilizes robotic arms controlled by the surgeon, offering enhanced precision and visualization.
- Abdominal Supracervical Hysterectomy: This involves a larger incision in the abdomen, similar to a C-section, to directly access and remove the uterus. This approach is less common for supracervical hysterectomy but may be necessary in complex cases.
The benefits of supracervical hysterectomy often include a potentially shorter hospital stay, quicker recovery time, and less postoperative pain compared to traditional abdominal total hysterectomy. Medical literature, including guidance from organizations like the American College of Obstetricians and Gynecologists (ACOG), suggests that supracervical hysterectomy, particularly when performed laparoscopically, may be associated with benefits such as shorter operating times and reduced blood loss compared to total hysterectomy. Additionally, some patients report a perception of maintained vaginal support and potentially better sexual function due to the preservation of the cervix.
Supracervical vs. Total Hysterectomy
The distinction between supracervical vs total hysterectomy lies primarily in whether the cervix is removed. Both procedures involve the removal of the uterus, but the implications of cervical preservation or removal are significant for patient care and follow-up. Understanding these differences is crucial when discussing surgical options with a healthcare provider.
| Feature | Supracervical Hysterectomy | Total Hysterectomy |
|---|---|---|
| Uterus Removal | Body of uterus removed | Entire uterus (body and cervix) removed |
| Cervix Status | Cervix preserved | Cervix removed |
| Cervical Cancer Screening | Required (Pap tests) | Generally not required (unless history of cervical dysplasia or specific circumstances) |
| Potential for Cyclic Bleeding | Small possibility of light cyclic bleeding (from cervical tissue) | No possibility of cyclic bleeding from the cervix |
| Pelvic Support | May help maintain natural pelvic floor support | May alter pelvic floor support, potentially affecting vaginal vault prolapse risk |
| Recovery Time | Potentially shorter, especially with minimally invasive approaches | Similar to supracervical, but may vary based on surgical approach and individual factors |
The choice between these two procedures depends on various factors, including the underlying medical condition, the presence of cervical abnormalities (such as a history of abnormal Pap smears or cervical cancer), and patient preference. For individuals with a healthy cervix and no history of cervical dysplasia, supracervical hysterectomy may be a viable option. However, if there is any concern about cervical pathology, a total hysterectomy is typically recommended to eliminate the risk of future cervical cancer.
