Retinoblastoma Stages
Understanding the retinoblastoma stages is crucial for effective diagnosis, treatment planning, and predicting outcomes for this rare eye cancer primarily affecting young children. Staging helps medical professionals determine the extent of the disease, guiding personalized care strategies.
Key Takeaways
- Retinoblastoma stages are determined using comprehensive evaluations, including eye exams and imaging.
- The International Classification of Intraocular Retinoblastoma (ICRB) categorizes tumors confined to the eye, primarily guiding eye-sparing treatments.
- The AJCC TNM Staging System for Retinoblastoma is a broader system that assesses tumor size, lymph node involvement, and metastasis, crucial for cases with potential extraocular spread.
- Early detection and accurate staging significantly influence treatment choices and improve the prognosis by retinoblastoma stage.
- Treatment strategies vary widely, from focal therapies for early-stage intraocular disease to chemotherapy and enucleation for more advanced cases.
What Are the Retinoblastoma Stages?
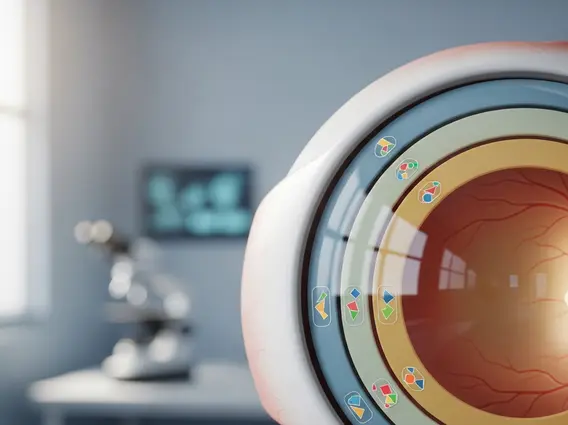
Retinoblastoma is a malignant tumor of the retina, the light-sensitive tissue at the back of the eye. To effectively treat this condition, medical professionals classify the disease into various retinoblastoma stages. This classification, also known as retinoblastoma tumor classification, provides a standardized way to describe the tumor’s size, location, and whether it has spread beyond the eye. Knowing what are the stages of retinoblastoma is fundamental because it directly impacts treatment decisions and the child’s long-term outlook.
There are primarily two widely accepted systems for staging retinoblastoma: the International Classification of Intraocular Retinoblastoma (ICRB) and the American Joint Committee on Cancer (AJCC) TNM staging system. Each system serves a distinct purpose, with ICRB focusing on tumors confined to the eye and TNM addressing both intraocular and extraocular disease.
International Classification of Intraocular Retinoblastoma (ICRB)
The International Classification of Intraocular Retinoblastoma (ICRB) is specifically designed for tumors that are contained within the eye. This system is critical for guiding treatment aimed at preserving the eye and vision. The retinoblastoma staging system explained by ICRB divides intraocular tumors into five groups (A through E), based on factors like tumor size, location relative to critical eye structures (such as the optic disc and fovea), and the presence of vitreous or subretinal seeding.
The ICRB helps clinicians assess the likelihood of successful eye preservation with various treatments. Generally, lower groups (A and B) have a higher chance of eye salvage, while higher groups (D and E) indicate more extensive disease, making eye preservation more challenging.
Group A: Small Tumors
Group A tumors represent the earliest and least extensive form of intraocular retinoblastoma. These are typically small tumors, measuring 3 millimeters or less in greatest dimension, and are located away from critical structures like the fovea (the center of vision) and the optic disc (where the optic nerve leaves the eye). Due to their small size and favorable location, Group A tumors have an excellent prognosis for eye preservation and vision, often treated with focal therapies such as laser photocoagulation or cryotherapy.
Group E: Extensive Tumors
In contrast, Group E tumors signify extensive intraocular retinoblastoma. These are large tumors that may involve significant portions of the retina, often extending close to or involving the optic disc or fovea. They are frequently associated with extensive vitreous or subretinal seeding, which indicates widespread tumor cells within the eye’s fluid or under the retina. Given the advanced nature of Group E tumors, the primary treatment often involves enucleation (surgical removal of the eye) to prevent extraocular spread and save the child’s life, though some cases might be considered for aggressive chemotherapy.
AJCC TNM Staging System for Retinoblastoma
The AJCC TNM Staging System for Retinoblastoma offers a more comprehensive framework, particularly when there is concern about the tumor spreading beyond the eye. This system, like other cancer staging systems, uses three main criteria: T for tumor (size and extent), N for nodes (involvement of regional lymph nodes), and M for metastasis (spread to distant parts of the body). This system helps define the different stages of retinoblastoma, from localized disease to distant metastasis.
The TNM system is vital for determining the overall prognosis and guiding systemic treatments, such as chemotherapy, especially when there’s evidence or suspicion of extraocular extension. It provides a detailed picture of the disease’s advancement, which is crucial for multidisciplinary treatment planning.
Pathological Staging
Pathological staging (pTNM) is determined after surgical removal of the eye (enucleation). This involves a microscopic examination of the removed eye and surrounding tissues by a pathologist. This detailed analysis can reveal crucial information, such as invasion of the optic nerve beyond the lamina cribrosa, choroidal invasion, or involvement of the sclera (the white outer layer of the eye). Pathological staging provides the most accurate assessment of the tumor’s extent and risk factors for recurrence or metastasis, which then informs the need for adjuvant therapies.
Clinical Staging
Clinical staging (cTNM) is performed before any definitive treatment, based on findings from a physical examination, imaging studies (such as MRI and ultrasound), and other diagnostic tests. This stage assesses the tumor’s size, location, and any visible signs of spread to the orbit or regional lymph nodes. Clinical staging helps in initial treatment planning, determining whether the tumor is confined to the eye or if there is evidence of extraocular extension, guiding decisions between eye-sparing therapies and enucleation, potentially followed by systemic treatment.
How Retinoblastoma Stages Are Determined
Determining how is retinoblastoma staged involves a thorough and multidisciplinary evaluation. The process typically begins with a comprehensive eye examination under anesthesia (EUA), allowing the ophthalmologist to visualize the retina and tumor(s) in detail. During the EUA, the doctor assesses the tumor’s size, number, location, and the presence of any vitreous or subretinal seeding.
Beyond the direct examination, several imaging techniques are crucial:
- Ocular Ultrasound: Helps measure tumor dimensions and detect calcifications, a common feature of retinoblastoma.
- Magnetic Resonance Imaging (MRI) of the Brain and Orbits: Essential for evaluating the extent of the tumor within the eye, assessing for optic nerve invasion, and detecting any spread to the brain or surrounding orbital tissues.
- Lumbar Puncture and Bone Marrow Biopsy: May be performed if there is suspicion of metastatic disease, though this is rare.
- Genetic Testing: Can identify mutations in the RB1 gene, which is important for understanding the risk of bilateral disease and for genetic counseling for the family.
The information gathered from these examinations and tests is collectively used to assign the appropriate ICRB group and AJCC TNM stage, providing a complete picture for understanding retinoblastoma stages.
Prognosis and Treatment by Retinoblastoma Stage
The prognosis by retinoblastoma stage is highly dependent on how early the cancer is detected and the extent of the disease at diagnosis. Retinoblastoma has one of the highest cure rates among childhood cancers, especially when diagnosed and treated early. According to the World Health Organization (WHO), retinoblastoma is curable in over 95% of cases if detected early and managed appropriately.
Treatment strategies are highly individualized and directly correlated with the assigned stage:
- Early Intraocular Disease (ICRB Group A, B, C): For smaller tumors confined to the eye, treatments often focus on preserving the eye and vision. These may include focal therapies such as laser photocoagulation, cryotherapy, or brachytherapy (placing a radioactive plaque on the eye). Systemic chemotherapy may also be used to shrink larger tumors before focal treatment or to treat multifocal disease.
- Advanced Intraocular Disease (ICRB Group D, E): For extensive tumors within the eye, especially those with significant seeding, the primary goal shifts to saving the child’s life. Enucleation (surgical removal of the eye) is frequently recommended to prevent the spread of cancer. In some cases, intra-arterial chemotherapy (IAC) or intravitreal chemotherapy (IViC) may be considered to avoid enucleation, particularly for Group D tumors.
- Extraocular Disease (AJCC TNM Stage II, III, IV): If the cancer has spread beyond the eye to the optic nerve, orbit, or distant sites, treatment becomes more aggressive. This typically involves enucleation, followed by systemic chemotherapy and sometimes external beam radiation therapy. The prognosis for extraocular retinoblastoma is less favorable than for intraocular disease, underscoring the importance of early detection and accurate staging.
Regular follow-up examinations are crucial after treatment to monitor for recurrence or the development of new tumors, especially in children with hereditary retinoblastoma.
Frequently Asked Questions
What is the main difference between ICRB and AJCC TNM staging systems?
The International Classification of Intraocular Retinoblastoma (ICRB) primarily focuses on tumors confined within the eye, categorizing them based on size, location, and seeding to guide eye-sparing treatments. In contrast, the AJCC TNM system is more comprehensive, assessing the tumor’s extent (T), involvement of regional lymph nodes (N), and distant metastasis (M). It is used for both intraocular and extraocular disease, providing a broader assessment of the cancer’s spread and overall prognosis, particularly for advanced cases.
Why is early detection critical for retinoblastoma?
Early detection of retinoblastoma is paramount because it significantly improves the chances of successful treatment, eye preservation, and saving the child’s life. When detected in its early stages (e.g., ICRB Group A or B), tumors are smaller and confined, allowing for less invasive, eye-sparing therapies with excellent visual outcomes. Conversely, delayed diagnosis can lead to larger tumors, extraocular spread, and a higher risk of metastasis, necessitating more aggressive treatments like enucleation and chemotherapy, with a less favorable prognosis.
Can retinoblastoma recur after treatment?
Yes, retinoblastoma can recur after treatment, although the risk varies depending on the initial stage and treatment method. Recurrence can manifest as new tumors in the treated eye, in the other eye (especially in hereditary cases), or as extraocular spread. Regular follow-up examinations under anesthesia are essential for several years after initial treatment to monitor for any signs of recurrence. Prompt detection of recurrence allows for timely intervention, which is critical for maintaining a high success rate in managing the disease.
