Intraoperative Radiation Therapy
Intraoperative Radiation Therapy (IORT) represents a specialized and advanced approach in cancer treatment, delivering a concentrated dose of radiation directly to the tumor site during surgery. This technique aims to maximize radiation efficacy while minimizing exposure to surrounding healthy tissues.
Key Takeaways
- IORT delivers a high dose of radiation directly to the tumor bed during surgery.
- It is often used for various cancers, including breast, colorectal, and pancreatic, among others.
- The procedure aims to reduce the number of radiation treatment sessions post-surgery.
- Benefits include precise targeting, reduced overall treatment time, and minimized side effects.
- IORT can improve local tumor control and potentially enhance patient outcomes.
What is Intraoperative Radiation Therapy (IORT)?
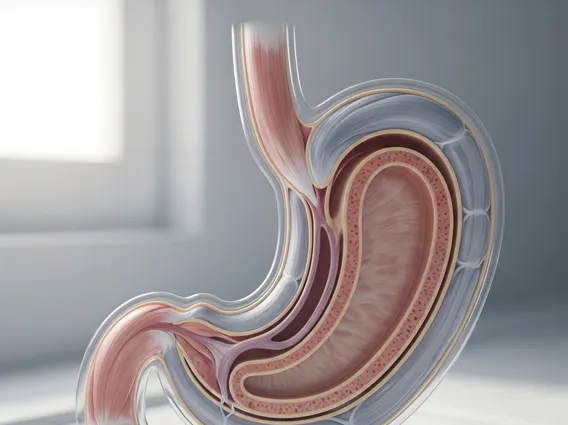
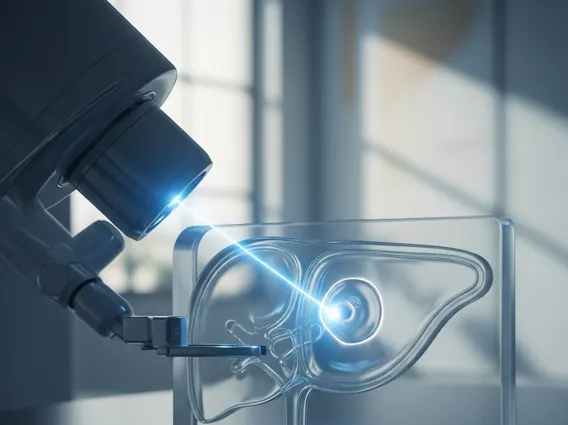
Intraoperative Radiation Therapy (IORT) is a highly specialized form of radiation treatment where a single, high dose of radiation is delivered directly to the tumor bed or residual tumor cells during a surgical procedure. This innovative approach allows radiation oncologists to target cancerous tissue with extreme precision immediately after its surgical removal, or to treat areas where complete removal is not possible. By administering radiation while the surgical site is open, healthy organs and tissues can be physically moved out of the radiation field, significantly reducing their exposure and potential damage. This direct application aims to eradicate microscopic disease that might remain after visible tumor removal, thereby reducing the risk of local recurrence.
IORT is typically performed in a specially equipped operating room, combining the expertise of surgical oncologists and radiation oncologists. The goal is to provide a potent, localized dose of radiation that might otherwise require multiple external beam radiation therapy sessions over several weeks. This method is particularly beneficial for certain types of cancer where precise targeting is crucial and minimizing radiation to adjacent critical structures is paramount.
The Intraoperative Radiation Therapy Procedure
The intraoperative radiation therapy procedure involves a carefully coordinated effort between the surgical and radiation oncology teams. Once the primary tumor has been surgically removed, or the area requiring treatment has been exposed, the radiation oncologist takes over. A specialized radiation delivery device, such as a linear accelerator or a portable electron beam unit, is brought into the operating room. The area to be treated is meticulously defined, and protective shields are often used to further safeguard surrounding healthy tissues and organs.
During the procedure, a single, high dose of radiation is delivered directly to the target area. The specific type of radiation and its energy level are chosen based on the tumor type, its location, and the patient’s overall treatment plan. This direct application ensures that the radiation penetrates only to the required depth, effectively treating the microscopic disease while sparing adjacent structures. After the radiation dose is administered, the surgical team completes the operation by closing the incision. The entire process, from tumor removal to radiation delivery and surgical closure, is typically completed in one surgical setting. This integrated approach is a key aspect of how intraoperative radiation therapy works, streamlining treatment and potentially reducing the overall duration of therapy.
Benefits of Intraoperative Radiation Therapy
The benefits of intraoperative radiation therapy are significant, offering several advantages over conventional external beam radiation therapy for select patients. One primary benefit is the ability to deliver a highly concentrated dose of radiation directly to the tumor bed, maximizing its effectiveness against residual cancer cells. This precision helps to minimize damage to nearby healthy organs and tissues, which can often be shielded or moved out of the radiation field during surgery.
- Enhanced Precision: Direct visualization during surgery allows for highly accurate targeting of the tumor bed, ensuring the radiation is delivered exactly where it’s needed.
- Reduced Treatment Time: Patients often require fewer, or sometimes no, additional external beam radiation therapy sessions post-surgery, significantly shortening the overall treatment course.
- Minimized Side Effects: By sparing healthy tissues, IORT can lead to fewer acute and long-term side effects compared to conventional radiation, improving patient quality of life.
- Improved Local Control: The high, single dose delivered directly to the surgical margin can be very effective in eradicating microscopic disease, potentially reducing local recurrence rates.
- Convenience: Combining surgery and radiation into one event can be more convenient for patients, reducing hospital visits and logistical burdens.
According to data from various oncology centers, IORT has shown promise in improving local control for certain cancers, contributing to better patient outcomes and potentially reducing the need for prolonged adjuvant therapies.