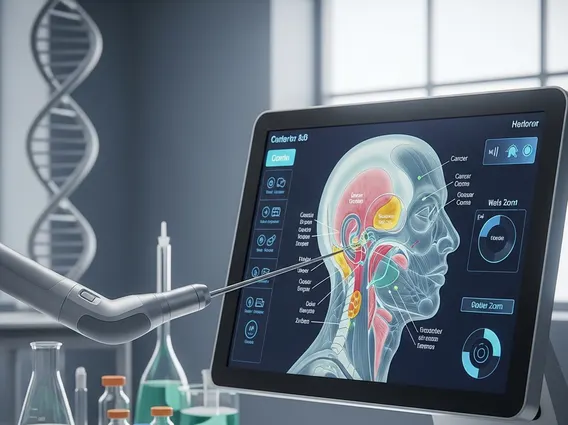
Head and Neck Cancer Treatment Options
Managing head and neck cancer involves informed decision-making regarding treatment planning and delivery. Therapeutic strategies are shaped by tumor location, disease severity, and individual health considerations. In some cases, a single therapy may be sufficient, while others need combined approaches to manage disease and protect vital functions.
Key Takeaways
- Head and neck cancer treatments often rely on a multimodal approach, where different therapies are strategically combined to address both tumor control and functional preservation.
- The most appropriate treatment for head and neck cancer is determined through careful evaluation of tumor characteristics, disease stage, and patient-specific health considerations.
- Therapeutic interventions are designed not only to manage the disease but also to maintain functional ability and daily quality of life whenever possible.
- Radiation and medication-based therapies may be used alone or together.
- Multidisciplinary care plays a central role in treatment planning.
Primary Treatment Approaches for Head and Neck Cancer
The primary goal of head and neck cancer treatment options is to eliminate or control cancer while minimizing functional impairment. Care planning is usually carried out by a collaborative team of specialists, bringing together expertise from surgical, medical, and radiation oncology.
Standard treatment strategies may involve tumor removal through surgery, localized radiation to address cancerous tissue, or systemic medications such as chemotherapy and targeted agents. In many cases, head and neck cancer medication is used alongside other treatments to improve effectiveness. Treatment plans are tailored to each patient and can be adjusted over time based on how the disease responds to ongoing therapy.
- Surgical intervention for localized tumors
- Radiation-based approaches, including head and neck radiation
- Systemic medication therapies
- Combined-modality treatment for advanced disease
Surgical Treatment and Medical Procedures for Head and Neck Cancer
Surgery remains a key head and neck cancer medical procedure, particularly for early-stage or localized tumors. The extent of surgery depends on tumor size and location, and modern techniques aim to preserve surrounding tissues whenever possible.
For more advanced disease, surgical treatment is often supported by additional therapies to help lower the likelihood of cancer returning. Surgical planning also considers reconstruction and rehabilitation needs, ensuring patients maintain essential functions after treatment. Treatment planning for head and neck cancer follows established clinical frameworks that compare available therapies based on goals, benefits, and potential risks.
| Treatment Type | Primary Purpose | Key Considerations |
|---|---|---|
| Surgery | Tumor removal | Functional preservation |
| Radiation Therapy | Target cancer cells | Side effect management |
| Systemic Medication | Treat cancer throughout the body | Requires monitoring |
| Combined Treatment | Improve disease control | Multidisciplinary planning |
Radiation Therapy in Head and Neck Cancer Care
Head and neck radiation plays a critical role in cancer care and may be applied as a standalone therapy or integrated with other treatment methods depending on clinical needs.
In certain cases, head and neck cancer radiation therapy is combined with systemic medication to enhance treatment effectiveness. Side effects vary depending on radiation dose and treatment area, making supportive care and monitoring an essential part of the process.
Radiation therapy may be administered following surgery to reduce recurrence risk, or used as a primary treatment option when surgical intervention is not appropriate. Side effects may include skin irritation, dry mouth, fatigue, or swallowing difficulties, which are managed through supportive care and close monitoring. Radiation treatment plans are individualized, taking tumor location and patient tolerance into account.
Systemic Therapies and Cancer Medication
Systemic treatment options for head and neck cancer consist of chemotherapy, targeted agents, and immunotherapy, all of which exert effects throughout the body. These therapies may be used at various points in care, including as neoadjuvant, adjuvant, or concurrent treatments with radiation. The selection of medication depends on tumor biology, overall health, and treatment goals. Patients are monitored closely throughout treatment to address side effects and modify therapy when necessary.
Systemic therapy can be delivered on its own or alongside radiation to improve treatment outcomes. Medication selection is influenced by tumor characteristics, therapeutic objectives, and the patient’s overall condition. Ongoing monitoring allows care teams to evaluate response and ensure treatment remains both safe and effective. When appropriately selected, systemic therapies contribute to comprehensive head and neck cancer treatment options.
Rehabilitation and Functional Recovery After Head and Neck Cancer Treatment
Recovery following head and neck cancer treatments often involves more than tumor control. Because the head and neck region plays a critical role in speaking, swallowing, and breathing, treatment may affect daily functions even when cancer control is successful. Rehabilitation focuses on restoring these functions and supporting long-term quality of life.
Patients may require speech and swallowing therapy, nutritional support, or physical rehabilitation depending on the treatment received. Recovery timelines vary, and progress is often gradual. Integrating rehabilitation early into the care plan allows patients to adapt more effectively and manage treatment-related changes. Functional recovery is considered an essential part of comprehensive treatment for head and neck cancer, not a separate phase of care.
Factors Influencing Treatment Selection and Outcomes in Head and Neck Cancer
Choosing among available head and neck cancer treatment options depends on several interrelated factors. Tumor location, disease stage, and biological characteristics guide clinical decision-making, while patient age, overall health, and functional priorities also play an important role. No single treatment approach is universally appropriate.
Outcomes are influenced by how well therapies are matched to individual needs and how effectively side effects are managed during treatment. Adherence to evidence-based care pathways and established head and neck cancer treatment guidelines helps optimize both disease control and long-term well-being. Ongoing evaluation allows care teams to adjust treatment strategies as needed, supporting safer and more personalized outcomes.
FAQ: Head and Neck Cancer Treatment Options
Is head and neck cancer curable?
The potential for curing head and neck cancer varies based on the specific cancer type, how early it is diagnosed, and how well it responds to treatment.
Early-stage cancers may be treated successfully, while advanced cases often focus on long-term disease control and quality of life. Treatment outcomes vary, and care teams tailor approaches to individual circumstances.
What are the most common head and neck cancer treatments?
In clinical practice, head and neck cancer treatments are tailored to each individual and may be adjusted over time as treatment response and patient tolerance are closely monitored.
Standard care for head and neck cancer may involve surgery, radiation therapy, and systemic treatments such as chemotherapy, targeted agents, or immunotherapy. These modalities are selected and combined based on tumor site, disease stage, and the patient’s general health, with an emphasis on maintaining functional outcomes.
How are head and neck cancer treatment options decided?
Selecting head and neck cancer treatment options involves evaluating tumor characteristics, imaging results, and patient-specific factors. Multidisciplinary teams follow evidence-based head and neck cancer treatment guidelines to determine the most appropriate sequence or combination of therapies. Ongoing assessment allows adjustments based on treatment response and side effects.
