Enteral Nutrition
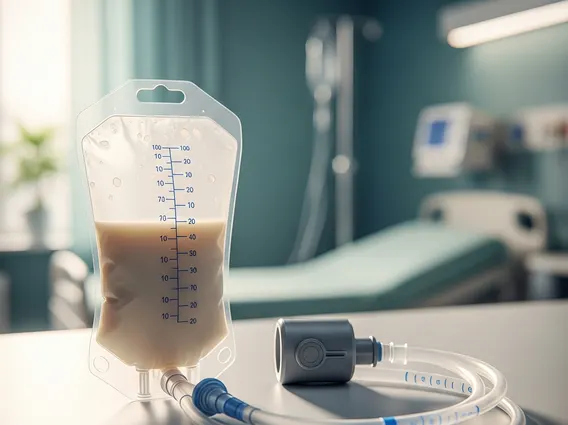
Enteral nutrition is a vital medical intervention for individuals unable to meet their nutritional needs through conventional oral intake. It involves delivering nutrient-rich formulas directly into the gastrointestinal tract, ensuring essential sustenance and supporting recovery and overall well-being.
Key Takeaways
- Enteral nutrition provides essential nutrients directly to the digestive system when oral intake is insufficient or impossible.
- It supports patient recovery, maintains gut function, and prevents malnutrition by delivering complete liquid formulas.
- Various feeding tubes, such as nasogastric, gastrostomy, and jejunostomy tubes, are used depending on the patient’s condition and anticipated duration of need.
- Proper management and care are crucial for preventing complications and optimizing patient outcomes, ensuring safe and effective nutritional support.
What is Enteral Nutrition?
Enteral Nutrition refers to the delivery of a nutritionally complete liquid formula directly into the stomach or small intestine through a tube. This method is employed when a person cannot eat or drink enough to maintain adequate nutrition, but their gastrointestinal (GI) tract is still functional. It is distinct from parenteral nutrition, which delivers nutrients intravenously. The primary goal of enteral nutrition definition is to provide essential calories, protein, vitamins, and minerals to support metabolic needs, promote healing, and prevent malnutrition. It is a critical component of care for patients with various conditions, including dysphagia (difficulty swallowing), critical illness, gastrointestinal disorders, neurological impairments, and certain types of cancer. This approach leverages the body’s natural digestive processes, which can offer several physiological advantages over intravenous feeding.
Benefits of Enteral Nutrition
The enteral nutrition benefits are numerous and contribute significantly to patient recovery and overall health outcomes. One of the primary advantages is the maintenance of gut integrity and function. By stimulating the gut with nutrients, enteral feeding helps prevent bacterial translocation from the gut into the bloodstream and preserves the natural barrier function of the intestines, which is crucial for immune health. This physiological stimulation also helps maintain the health of the gut microbiota. Compared to parenteral nutrition, enteral nutrition is generally associated with fewer complications, such as infections, and is often more cost-effective, reducing the overall burden on healthcare systems. It also supports better glycemic control in critically ill patients, which is vital for reducing morbidity and mortality.
- Maintains Gut Health: Preserves the structure and function of the intestinal lining, reducing the risk of complications like gut atrophy and promoting a healthy gut microbiome.
- Reduces Infection Risk: Lower incidence of bloodstream infections and other systemic infections compared to intravenous feeding, due to preserved gut barrier function.
- Improved Immune Function: Supports the gut-associated lymphoid tissue (GALT), a critical part of the immune system, enhancing the body’s defense mechanisms.
- Better Nutrient Utilization: Mimics physiological digestion and absorption more closely than intravenous methods, leading to more efficient nutrient uptake.
- Cost-Effectiveness: Generally less expensive than parenteral nutrition, reducing healthcare costs and resource utilization without compromising care quality.
Types of Enteral Feeding Tubes
There are several enteral feeding tube types, each designed for specific patient needs and anticipated durations of use. The choice of tube depends on factors such as the anticipated length of feeding, the patient’s gastrointestinal function, the risk of aspiration (inhaling food or liquid into the lungs), and the patient’s overall medical condition.
- Nasogastric (NG) Tube: This tube is inserted through the nose, down the esophagus, and into the stomach. It is typically used for short-term feeding (generally less than 4-6 weeks) and is relatively easy to place and remove, making it a common initial choice.
- Nasojejunal (NJ) Tube: Similar to an NG tube, but it extends past the stomach into the jejunum (the middle part of the small intestine). This type is often used for patients with gastric motility issues, severe gastroesophageal reflux, or a high risk of aspiration, as it bypasses the stomach.
- Gastrostomy Tube (G-tube): A tube inserted directly into the stomach through a small surgical opening in the abdominal wall. G-tubes are suitable for long-term feeding (more than 4-6 weeks) and can be discreetly managed under clothing. Percutaneous endoscopic gastrostomy (PEG) is a common, minimally invasive method for placing G-tubes.
- Jejunostomy Tube (J-tube): This tube is surgically placed directly into the jejunum. J-tubes are used for long-term feeding when the stomach needs to be completely bypassed, such as in cases of severe gastroparesis (delayed stomach emptying), gastric outlet obstruction, or when there is an unmanageable high risk of aspiration that cannot be addressed by an NJ tube.
Each type requires careful placement, meticulous management, and comprehensive patient and caregiver education to ensure safety and efficacy. Regular monitoring by healthcare professionals is essential to prevent complications, ensure proper tube function, and optimize nutritional support for the patient.
