Diagnosis, Screening, and Early Detection of Tongue Cancer
Tongue cancer, a form of oral cancer, can be life-threatening if not detected and treated early. Understanding its signs, available screening methods, and the diagnostic process is crucial for improving patient outcomes.
Key Takeaways
- Early recognition of symptoms like persistent sores, pain, or difficulty swallowing is vital for prompt medical consultation.
- Regular oral cancer screenings, especially for individuals with risk factors, can significantly aid in the early detection of tongue cancer.
- The definitive diagnosis of tongue cancer involves a biopsy, followed by imaging tests to determine the cancer’s extent.
- Understanding the TNM staging system helps classify the cancer’s progression, which is critical for guiding treatment decisions.
- Proactive awareness and timely medical intervention are key to effective management and improved prognosis for tongue cancer.
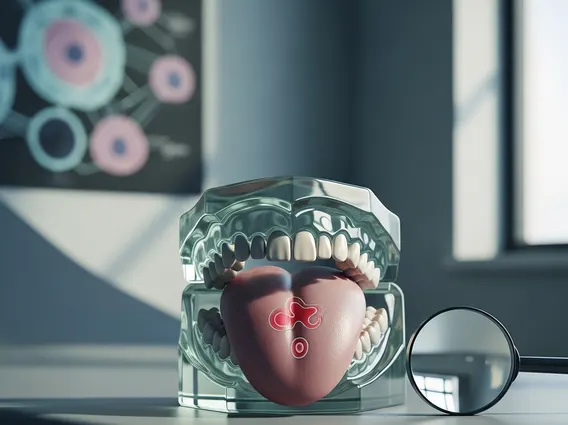
Recognizing Early Signs of Tongue Cancer
Identifying the early signs of tongue cancer is paramount for timely intervention and improved prognosis. Many symptoms can be subtle initially, often mimicking less serious conditions, making awareness critical.
Common Visual and Physical Symptoms
The symptoms of early tongue cancer can manifest in various ways, often starting as a persistent change on the tongue. These may include:
- Persistent Sore or Ulcer: A sore on the tongue that does not heal within two weeks is a primary warning sign. Unlike common canker sores, these often do not resolve and may gradually enlarge.
- Red or White Patches: Erythroplakia (red patches) or leukoplakia (white patches) on the tongue’s surface can be precancerous lesions. While not all patches are cancerous, any persistent, unexplained patch warrants investigation.
- Pain or Numbness: Persistent pain in the tongue, throat, or ear, or a feeling of numbness in parts of the mouth, can indicate underlying issues. This pain may worsen with eating or speaking.
- Difficulty Swallowing or Chewing: As the tumor grows, it can interfere with normal tongue movement, leading to dysphagia (difficulty swallowing) or discomfort while chewing.
- Lump or Thickening: A noticeable lump, thickening, or hardened area on the tongue that wasn’t previously present.
- Bleeding: Unexplained bleeding from the tongue, especially without injury, should prompt medical attention.
According to the American Cancer Society, oral cavity and oropharyngeal cancers, which include tongue cancer, are estimated to affect over 54,000 people in the United States in 2024. Early detection significantly improves the 5-year survival rate for localized disease, which can be as high as 85% for oral cavity cancers. (Source: American Cancer Society, “Key Statistics for Oral Cavity and Oropharyngeal Cancers”, “Survival Rates for Oral Cavity and Oropharyngeal Cancers”)
When to Seek Medical Attention
It is crucial to seek medical attention if any of the aforementioned symptoms persist for more than two weeks. While many oral lesions are benign, only a healthcare professional can accurately assess the situation. Delaying consultation can allow cancer to progress, making treatment more complex and potentially less effective. Regular self-examinations of the mouth and tongue can also help individuals identify changes early.
Screening Methods for Early Detection
Proactive screening plays a pivotal role in the early detection of tongue cancer, particularly for individuals at higher risk. These screenings are often integrated into routine dental and medical check-ups.
Oral Cancer Screenings
The primary screening methods for tongue cancer involve a thorough visual and tactile examination of the entire oral cavity, including the tongue, by a dentist or physician. During this examination, the healthcare provider will:
- Visually Inspect: Look for any asymmetry, swelling, lumps, bumps, ulcerations, or color changes (red, white, or dark patches) on the tongue, floor of the mouth, cheeks, gums, and palate.
- Palpate: Gently feel the tissues of the mouth, including the tongue and neck, to detect any unusual lumps, tenderness, or hardened areas that may not be visible.
- Review Medical History: Discuss any persistent symptoms the patient may be experiencing, such as pain, difficulty swallowing, or changes in taste.
These screenings are quick, non-invasive, and can identify suspicious areas that warrant further investigation. While there are no specific national screening programs solely for tongue cancer, these comprehensive oral examinations are considered standard practice for detecting various oral cancers.
High-Risk Factors and Targeted Screening
Certain factors significantly increase an individual’s risk of developing tongue cancer, necessitating more vigilant screening. These high-risk factors include:
- Tobacco Use: Smoking cigarettes, cigars, pipes, and using smokeless tobacco products are major risk factors.
- Alcohol Consumption: Heavy and prolonged alcohol use, especially when combined with tobacco, dramatically increases risk.
- Human Papillomavirus (HPV) Infection: Certain strains of HPV, particularly HPV-16, are linked to an increasing number of oral cancers, including those affecting the base of the tongue.
- Sun Exposure: While more common for lip cancer, prolonged sun exposure can also contribute to oral cancers.
- Poor Nutrition: A diet lacking in fruits and vegetables may increase risk.
For individuals with these risk factors, healthcare providers may recommend more frequent oral cancer screenings. Adherence to tongue cancer detection guidelines often means annual or even semi-annual examinations, allowing for the earliest possible identification of any suspicious lesions. Early detection in high-risk groups is crucial, as these individuals may develop cancer without prominent symptoms until it has advanced.
The Tongue Cancer Diagnosis Process
When suspicious lesions or symptoms are identified, a definitive tongue cancer diagnosis process begins. This typically involves a series of examinations and tests to confirm the presence of cancer and determine its extent.
Initial Examination and Biopsy
The initial step in how is tongue cancer diagnosed involves a thorough clinical examination by an oral surgeon, otolaryngologist (ENT specialist), or oncologist. This examination will meticulously assess the suspicious area, noting its size, location, texture, and any associated symptoms. The most crucial diagnostic step is the biopsy.
A biopsy involves taking a small tissue sample from the suspicious lesion. This procedure can be performed in several ways:
- Incisional Biopsy: A small piece of the abnormal tissue is surgically removed.
- Excisional Biopsy: The entire suspicious lesion is removed, if small enough, along with a margin of healthy tissue.
- Brush Biopsy: A small brush is used to collect cells from the surface of the lesion. While less invasive, it may require a follow-up incisional biopsy if abnormal cells are found.
The collected tissue is then sent to a pathologist, who examines it under a microscope to determine if cancer cells are present. This pathological analysis is the only definitive way to confirm a diagnosis of tongue cancer.
Imaging and Further Tests
Once cancer is confirmed, further tests are conducted to determine the cancer’s stage and whether it has spread. These imaging and diagnostic tests help the medical team understand the full extent of the disease:
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the head and neck, helping to assess the tumor’s size, its invasion into surrounding tissues, and potential spread to lymph nodes.
- Magnetic Resonance Imaging (MRI): Offers excellent soft tissue contrast, making it particularly useful for evaluating the extent of tumor invasion into the tongue muscle and surrounding structures, as well as detecting nerve involvement.
- Positron Emission Tomography (PET) Scan: Often combined with a CT scan (PET-CT), this scan can detect metabolically active cancer cells throughout the body, identifying distant metastases or involvement of lymph nodes not visible on other scans.
- Endoscopy: Procedures like laryngoscopy or esophagoscopy may be performed to check for other cancers in the upper aerodigestive tract, which can sometimes occur concurrently with oral cancer.
These tests collectively provide a comprehensive picture of the cancer, which is essential for accurate staging and treatment planning.
Understanding Tongue Cancer Stages
After diagnosis, determining what are the stages of tongue cancer is a critical step. Staging helps classify the cancer’s extent, guiding treatment decisions and providing an indication of prognosis.
TNM Staging System Explained
The most widely used system for staging tongue cancer, like most cancers, is the TNM system, developed by the American Joint Committee on Cancer (AJCC). TNM stands for:
- T (Tumor): Describes the size and extent of the primary tumor.
- T1: Tumor is 2 cm or less in greatest dimension.
- T2: Tumor is more than 2 cm but not more than 4 cm.
- T3: Tumor is more than 4 cm.
- T4: Tumor has invaded adjacent structures (e.g., bone, deep muscle of the tongue, skin).
- N (Nodes): Indicates whether the cancer has spread to nearby lymph nodes.
- N0: No regional lymph node metastasis.
- N1: Metastasis in a single ipsilateral lymph node, 3 cm or less.
- N2: Metastasis in a single ipsilateral lymph node, more than 3 cm but not more than 6 cm; or multiple ipsilateral lymph nodes, none more than 6 cm; or bilateral or contralateral lymph nodes, none more than 6 cm.
- N3: Metastasis in a lymph node more than 6 cm.
- M (Metastasis): Denotes whether the cancer has spread to distant parts of the body (e.g., lungs, liver, bones).
- M0: No distant metastasis.
- M1: Distant metastasis present.
These T, N, and M categories are then combined to assign an overall stage, typically ranging from Stage 0 (carcinoma in situ) to Stage IV (advanced cancer with distant metastasis).
Why Staging Matters for Treatment
The stage of tongue cancer is a crucial factor in determining the most appropriate and effective treatment plan. For instance:
- Early-stage cancers (Stage I and II): Often treated with surgery alone, or sometimes radiation therapy. The goal is typically to remove the tumor completely with minimal impact on function.
- Locally advanced cancers (Stage III and IVA): May require a combination of surgery, radiation therapy, and chemotherapy. The treatment aims to control the local disease and prevent regional spread.
- Metastatic cancers (Stage IVB): Treatment focuses on managing symptoms, improving quality of life, and extending survival, often involving systemic therapies like chemotherapy, targeted therapy, or immunotherapy.
Staging also provides valuable prognostic information, helping patients and their families understand the likely course of the disease and potential outcomes. Accurate staging ensures that patients receive tailored care, optimizing their chances for successful treatment and recovery.
Frequently Asked Questions
What is the most common symptom of early tongue cancer?
The most common early symptom of tongue cancer is a persistent sore or ulcer on the tongue that does not heal within two weeks. This lesion may be accompanied by pain, numbness, or a feeling of a lump. Unlike common canker sores, these cancerous lesions tend to persist and may gradually increase in size, often appearing as red or white patches. Any such persistent change warrants immediate medical evaluation.
How often should I get screened for tongue cancer?
For individuals with no significant risk factors, a routine oral cancer screening is typically part of an annual dental check-up. However, if you have high-risk factors such as a history of heavy tobacco and alcohol use, or HPV infection, your dentist or doctor may recommend more frequent screenings, possibly every six months. Regular self-examinations are also encouraged to detect any changes between professional screenings.
Can tongue cancer be cured if caught early?
Yes, tongue cancer has a significantly higher chance of being cured if detected and treated in its early stages. For localized oral cavity cancers, the 5-year survival rate can be as high as 85%. Early detection allows for less invasive treatment options, such as surgery alone, which can lead to better functional outcomes and a higher likelihood of complete remission. Prompt action upon noticing symptoms is critical.
