Diagnosis, Screening, and Early Detection of Hypopharyngeal Cancer
Hypopharyngeal cancer, a relatively rare but aggressive form of head and neck cancer, originates in the hypopharynx, the bottom part of the throat. Understanding its diagnosis, screening, and early detection is crucial for improving patient outcomes and survival rates.
Key Takeaways
- Early symptoms like persistent sore throat, difficulty swallowing, and voice changes warrant prompt medical evaluation.
- Individuals with significant risk factors, such as heavy smoking and alcohol consumption, are prime candidates for targeted screening efforts.
- Hypopharyngeal cancer diagnosis methods typically involve initial examinations, imaging (CT, MRI, PET), and definitive biopsy.
- Early detection of hypopharyngeal cancer significantly enhances treatment efficacy and patient prognosis.
- Regular check-ups for high-risk individuals are vital, as general population screening is not currently recommended.
Recognizing Early Symptoms of Hypopharyngeal Cancer
Identifying the subtle initial signs of hypopharyngeal cancer is often challenging, as symptoms can be non-specific and easily mistaken for common ailments. However, persistent or worsening symptoms should raise suspicion and prompt medical consultation. Recognizing these symptoms of hypopharyngeal cancer early signs is the first step towards timely intervention.
Common Warning Signs to Watch For
The hypopharynx plays a vital role in both breathing and swallowing, so early symptoms often relate to these functions. Patients may experience a range of discomforts that, when persistent, signal a potential issue. These include:
- Persistent Sore Throat: A sore throat that does not improve with standard remedies or lasts for several weeks.
- Difficulty Swallowing (Dysphagia): A sensation of food getting stuck in the throat or pain when swallowing, which can progressively worsen.
- Voice Changes: Hoarseness or a change in voice quality that persists for more than two weeks, indicating potential irritation or involvement of nearby vocal cords.
- Ear Pain: Referred pain to the ear (otalgia), especially on one side, without any obvious ear infection.
- Lump in the Neck: A palpable mass or swelling in the neck area, which could indicate enlarged lymph nodes due to cancer spread.
- Unexplained Weight Loss: Significant and unintentional weight loss, often due to difficulty eating or the body’s metabolic response to cancer.
- Difficulty Breathing: In advanced stages, a tumor can obstruct the airway, leading to shortness of breath.
When to Seek Medical Attention
While many of these symptoms can be caused by less serious conditions, their persistence or combination warrants immediate medical evaluation. If any of these signs last for more than two weeks, particularly in individuals with risk factors, it is crucial to consult a healthcare professional. Prompt medical attention can lead to an earlier hypopharyngeal cancer diagnosis, which is critical for effective treatment.
Screening and Risk Factors for Hypopharyngeal Cancer
Unlike some other cancers, there is no routine population-wide screening program for hypopharyngeal cancer due to its relative rarity and the lack of highly effective, non-invasive screening tools. However, understanding and identifying high-risk individuals is paramount for targeted surveillance and early intervention, emphasizing the importance of early hypopharyngeal cancer screening in specific populations.
Identifying High-Risk Individuals
Several factors significantly increase an individual’s risk of developing hypopharyngeal cancer. These risk factors are crucial for guiding clinical suspicion and determining who might benefit most from closer monitoring. Key risk factors include:
- Tobacco Use: Smoking cigarettes, cigars, or pipes, and using smokeless tobacco, is the strongest risk factor. According to the American Cancer Society, tobacco use is linked to about 85% of head and neck cancers.
- Heavy Alcohol Consumption: Chronic and heavy alcohol intake, especially when combined with tobacco use, dramatically increases risk. The synergistic effect of alcohol and tobacco is well-documented.
- Human Papillomavirus (HPV) Infection: While more commonly associated with oropharyngeal cancers, certain strains of HPV can also contribute to hypopharyngeal cancer development.
- Nutritional Deficiencies: Poor nutrition, particularly iron deficiency (e.g., Plummer-Vinson syndrome), has been linked to an increased risk.
- Exposure to Certain Chemicals: Occupational exposure to substances like asbestos or wood dust may also elevate risk.
Focusing on individuals with these risk factors is key to effective screening for hypopharyngeal cancer risks, allowing for more proactive health management.
Current Screening Approaches
For the general population, no specific screening tests are recommended. However, for individuals identified as high-risk, a proactive approach involves regular medical check-ups that include a thorough examination of the head and neck. This might involve:
- Clinical Examination: A doctor visually inspects the throat and neck, and palpates for any lumps or abnormalities.
- Indirect Laryngoscopy: Using a small mirror and a light, or a flexible fiber-optic scope (nasopharyngoscope), a specialist can examine the hypopharynx and surrounding structures.
These approaches are not true screening tests in the sense of detecting cancer before symptoms appear, but rather enhanced surveillance methods for those at elevated risk. The goal is to detect any changes or early signs of disease as promptly as possible, highlighting the critical role of vigilance in early detection of hypopharyngeal cancer among vulnerable groups.
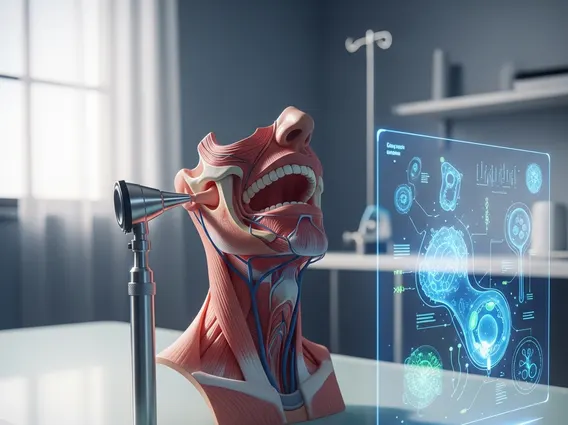
Key Methods for Hypopharyngeal Cancer Diagnosis
When symptoms suggest the possibility of hypopharyngeal cancer, a systematic diagnostic process is initiated to confirm the presence of cancer, determine its type, and assess its extent. This comprehensive approach ensures an accurate hypopharyngeal cancer diagnosis, which is vital for planning effective treatment strategies. Understanding how to diagnose hypopharyngeal cancer involves a series of specialized examinations and tests.
Initial Examinations and Imaging
The diagnostic journey typically begins with a detailed medical history and physical examination. If suspicion remains, further investigations are pursued:
- Direct Laryngoscopy and Pharyngoscopy: This procedure involves inserting a rigid or flexible scope directly into the throat under local or general anesthesia to get a magnified, detailed view of the hypopharynx. This allows the specialist to identify suspicious areas and often take biopsies.
- Imaging Studies: Advanced imaging techniques are crucial for visualizing the tumor, assessing its size, location, and whether it has spread to surrounding tissues or lymph nodes.
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the head and neck, helping to define tumor extent and lymph node involvement.
- Magnetic Resonance Imaging (MRI): Offers excellent soft tissue contrast, which is particularly useful for evaluating tumor invasion into muscles, nerves, and blood vessels.
- Positron Emission Tomography (PET) Scan: Often combined with CT (PET-CT), this scan helps identify metabolically active cancer cells throughout the body, useful for detecting distant metastasis or identifying the primary tumor if it’s unknown.
These initial steps are fundamental among the various hypopharyngeal cancer diagnosis methods, providing crucial information before a definitive diagnosis can be made.
Biopsy and Pathology Confirmation
The definitive diagnosis of hypopharyngeal cancer relies on a biopsy, which involves taking a small tissue sample from the suspicious area for microscopic examination. This is the gold standard for what is hypopharyngeal cancer detection:
- Biopsy: During direct laryngoscopy or pharyngoscopy, the surgeon removes a small piece of tissue from any abnormal-looking areas. This can also be done using fine-needle aspiration (FNA) for suspicious neck lumps.
- Pathology Examination: A pathologist examines the tissue under a microscope to confirm the presence of cancer cells, determine the specific type of cancer (most commonly squamous cell carcinoma), and assess its grade (how aggressive it appears).
Once cancer is confirmed, further tests may be conducted to stage the cancer, which involves determining the size of the tumor, whether it has spread to lymph nodes, and if it has metastasized to distant organs. This comprehensive diagnostic process is essential for accurate staging and guiding treatment decisions.
The Critical Role of Early Detection
The prognosis for hypopharyngeal cancer is significantly influenced by the stage at which it is diagnosed. Due to its aggressive nature and tendency to spread early, early detection of hypopharyngeal cancer is not just beneficial but absolutely critical for improving patient outcomes. This underscores the importance of early hypopharyngeal cancer screening, especially for at-risk populations.
Impact on Treatment Outcomes
When hypopharyngeal cancer is detected at an early stage, typically when the tumor is small and localized, the range of treatment options available is broader, and their efficacy is significantly higher. Early-stage cancers are more amenable to curative treatments such as surgery, radiation therapy, or a combination of both, often with less aggressive interventions. For instance, localized tumors might be removed with less extensive surgery, preserving more of the patient’s swallowing and speaking functions. Conversely, advanced-stage cancers often require more complex and aggressive treatments, including extensive surgery, higher doses of radiation, and chemotherapy, which can lead to more severe side effects and a diminished quality of life. According to the National Cancer Institute, the 5-year survival rate for localized hypopharyngeal cancer is significantly higher than for regional or distant disease.
Improving Patient Prognosis
The direct correlation between early diagnosis and improved survival rates cannot be overstated. Patients whose cancer is detected early have a much better chance of achieving long-term remission and a higher overall survival rate. Early diagnosis allows for prompt initiation of treatment before the cancer has had a chance to spread extensively to lymph nodes or distant organs, which are hallmarks of advanced disease. Furthermore, early detection can lead to treatments that are less debilitating, helping to preserve vital functions like speech and swallowing, thereby enhancing the patient’s quality of life post-treatment. This emphasizes why understanding what is hypopharyngeal cancer detection and acting on early symptoms is paramount for a favorable prognosis.
Frequently Asked Questions
What are the primary risk factors for hypopharyngeal cancer?
The most significant risk factors for hypopharyngeal cancer are heavy tobacco use, including smoking and smokeless tobacco, and chronic, excessive alcohol consumption. These two factors often act synergistically, greatly increasing risk. Other contributing factors can include certain strains of Human Papillomavirus (HPV), poor nutrition, and specific genetic predispositions. Individuals with a combination of these risk factors should be particularly vigilant about potential symptoms and discuss screening with their healthcare provider.
How effective are current screening methods for hypopharyngeal cancer?
Currently, there are no universally recommended population-wide screening programs for hypopharyngeal cancer due to its relative rarity and the lack of highly effective, non-invasive tests for asymptomatic individuals. However, for high-risk individuals (e.g., heavy smokers/drinkers), regular clinical examinations and indirect laryngoscopy serve as important surveillance tools. While not true “screening” in the traditional sense, these methods can aid in the early detection of hypopharyngeal cancer by identifying suspicious changes promptly, improving the chances of a favorable outcome.
Why is early detection so crucial for this type of cancer?
Early detection is paramount for hypopharyngeal cancer because it is an aggressive cancer that often spreads quickly to lymph nodes and other parts of the body. When detected at an early, localized stage, treatment options are more effective, less invasive, and carry a significantly higher chance of cure and long-term survival. Conversely, advanced-stage diagnoses often necessitate more aggressive treatments, leading to poorer prognoses and a greater impact on quality of life. Therefore, prompt recognition of symptoms and timely diagnosis are critical for improving patient outcomes.
