Scatter Radiation
Scatter Radiation is an unavoidable byproduct in medical imaging that significantly impacts image quality and patient and staff safety. Understanding its nature and methods of mitigation is crucial for accurate diagnosis and effective radiation protection.
Key Takeaways
- Scatter Radiation originates when X-ray photons interact with the patient’s body and change direction.
- It degrades image quality by introducing unwanted noise and reducing contrast, making diagnostic interpretation challenging.
- The amount of scatter produced is influenced by factors such as X-ray beam energy (kVp), field size, and patient thickness.
- Effective strategies to minimize scatter include collimation, using anti-scatter grids, and employing the air gap technique.
- Reducing scatter not only improves image clarity but also contributes to lower radiation exposure for patients and medical personnel.
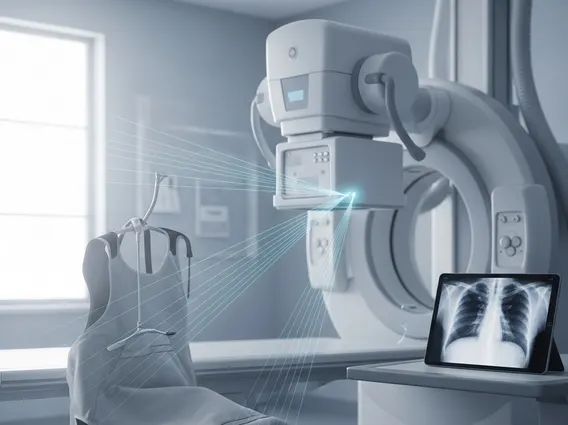
What is Scatter Radiation in Medical Imaging?
Scatter Radiation refers to the secondary radiation produced when primary X-ray photons interact with matter, such as the patient’s tissues, and deviate from their original path. This phenomenon is a fundamental aspect of X-ray physics and is particularly prevalent in diagnostic medical imaging procedures. The primary mechanism responsible for the generation of scatter radiation is Compton scattering, where an incident X-ray photon interacts with an outer-shell electron of an atom, imparting some of its energy to the electron and changing its direction.
The scatter radiation definition and causes are rooted in these interactions within the patient’s body. Factors that increase the likelihood and amount of scatter include higher kilovoltage peak (kVp) settings, which result in more energetic photons capable of Compton scattering; larger field sizes, as more tissue volume is irradiated; and increased patient thickness or density, providing more material for photons to interact with. This scattered radiation travels in random directions, with a significant portion reaching the image receptor, where it can obscure diagnostic information.
Effects of Scatter Radiation on Image Quality
The presence of Scatter Radiation has several detrimental effects on the quality of medical images, directly impacting diagnostic accuracy. When scattered photons reach the image receptor, they contribute to the overall signal without conveying specific anatomical information from the region of interest. This random, non-image-forming radiation effectively acts as a form of “fog” on the image.
One of the most significant consequences is the degradation of image contrast. Contrast is the difference in signal intensity between adjacent tissues or structures. Scatter radiation uniformly increases the background signal across the image, reducing the relative difference between areas of varying absorption. This makes it harder to distinguish subtle tissue variations, such as early lesions or fine anatomical details. Furthermore, scatter contributes to increased image noise, which refers to random fluctuations in signal intensity that obscure fine details and make the image appear grainy. The cumulative effect of reduced contrast and increased noise is a less clear, less diagnostic image, potentially leading to misinterpretations or the need for repeat examinations, thereby increasing patient radiation dose.
Methods to Reduce Scatter Radiation Exposure
Minimizing Scatter Radiation is a critical objective in medical imaging to enhance image quality and reduce unnecessary radiation exposure for both patients and healthcare professionals. Several effective techniques are employed:
- Collimation: This involves restricting the X-ray beam to the smallest possible area of interest. By reducing the volume of irradiated tissue, fewer photons are available to undergo Compton scattering, thereby decreasing the amount of scatter produced.
- Anti-Scatter Grids: These devices are placed between the patient and the image receptor. Grids consist of thin lead strips separated by radiolucent interspace material (e.g., aluminum or fiber). They are designed to absorb scattered photons traveling at oblique angles, allowing primary, image-forming photons to pass through to the detector.
- Air Gap Technique: This method involves increasing the distance between the patient and the image receptor. Since scattered photons travel in divergent paths, a larger air gap allows more scattered photons to diverge away from the detector before reaching it, while primary photons continue in a relatively straight line.
- Patient Compression: Applying compression to the patient can reduce the thickness of the body part being imaged. A thinner body part means less tissue for X-ray photons to interact with, consequently reducing the production of scatter radiation.
- Optimal kVp Selection: While higher kVp generally increases the proportion of Compton scattering, careful selection of the lowest appropriate kVp for a given examination can sometimes help manage scatter, balancing penetration with scatter production.
Implementing these methods effectively is essential for optimizing image quality, ensuring diagnostic accuracy, and upholding radiation safety standards in medical imaging practices.