Pancreatoduodenectomy
Pancreatoduodenectomy is a highly complex surgical procedure primarily performed to remove tumors from the head of the pancreas, duodenum, common bile duct, or ampulla of Vater. It is a major operation requiring significant expertise and is often a life-saving intervention for certain cancers and conditions.
Key Takeaways
- Pancreatoduodenectomy is a complex surgery involving the removal of parts of the pancreas, duodenum, gallbladder, and bile duct.
- It is primarily performed to treat cancers of the pancreas, bile duct, duodenum, and ampulla of Vater.
- The procedure carries significant risks, including pancreatic fistula, bleeding, and infection, with morbidity rates ranging from 30% to 50%.
- Recovery is extensive, requiring a prolonged hospital stay, careful pain management, and dietary adjustments.
- Long-term follow-up is crucial for managing potential complications like diabetes and malabsorption.
What is Pancreatoduodenectomy?
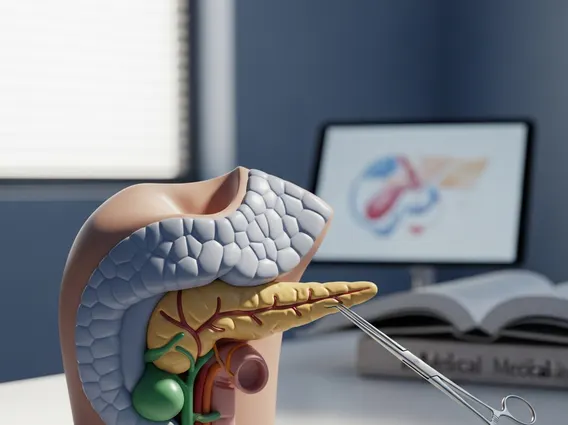
Pancreatoduodenectomy refers to a major surgical operation that involves the removal of the head of the pancreas, the duodenum (the first part of the small intestine), the gallbladder, and a portion of the common bile duct. This intricate procedure is most commonly known as the Whipple procedure, named after American surgeon Allen Oldfather Whipple. It is typically performed to treat malignant tumors in these areas, such as pancreatic cancer, duodenal cancer, cholangiocarcinoma (bile duct cancer), and ampullary cancer, as well as certain benign conditions or cysts that pose a risk of malignancy. Due to its complexity and the vital organs involved, it is considered one of the most challenging abdominal surgeries.
Pancreatoduodenectomy Procedure and Associated Risks
The **pancreatoduodenectomy procedure explained** involves several critical steps. Initially, the surgeon meticulously removes the diseased parts: the head of the pancreas, the entire duodenum, a portion of the jejunum (the middle part of the small intestine), the gallbladder, and the common bile duct. After these resections, the remaining digestive organs are carefully reconnected to restore the flow of bile, pancreatic enzymes, and food through the digestive tract. This reconstruction typically involves connecting the remaining pancreas to the jejunum, the bile duct to the jejunum, and the stomach to the jejunum. The duration of the surgery can vary but often takes several hours.
Despite advancements in surgical techniques and perioperative care, the **risks of pancreatoduodenectomy operation** are considerable. While surgical mortality rates have significantly decreased in high-volume centers, often falling below 5%, the morbidity rates remain substantial. According to data from the American College of Surgeons, complications can affect 30% to 50% of patients. Common risks include:
- Pancreatic fistula: A leakage of pancreatic fluid from the surgical connections, which can lead to infection and other serious complications.
- Bleeding: Hemorrhage can occur during or after the surgery, sometimes requiring blood transfusions or further intervention.
- Infection: Surgical site infections or intra-abdominal infections are possible.
- Delayed gastric emptying: The stomach may take longer than usual to empty, leading to nausea, vomiting, and difficulty eating.
- Bile leak: Leakage from the bile duct connections.
- Malabsorption: Difficulty absorbing nutrients due to changes in the digestive system.
Patients are thoroughly evaluated before surgery to assess their overall health and ability to withstand such a major operation, and a multidisciplinary team works to minimize these risks.
Recovery After Pancreatoduodenectomy Surgery
The **recovery after pancreatoduodenectomy surgery** is a prolonged and challenging process. Patients typically remain in the hospital for 1 to 3 weeks, often starting in an intensive care unit (ICU) for close monitoring. Pain management is a critical aspect of initial recovery, often involving intravenous medications and epidural catheters. Gradually, patients are encouraged to ambulate and begin a clear liquid diet, progressing to soft foods as tolerated. Nutritional support, sometimes through a feeding tube, may be necessary if the patient struggles to eat sufficiently.
Upon discharge, continued recovery at home can take several weeks to months. Patients may experience fatigue, changes in bowel habits, and difficulty with digestion. Long-term considerations often include managing pancreatic enzyme insufficiency, which may require enzyme supplements, and monitoring for new-onset diabetes or worsening existing diabetes, as a portion of the pancreas responsible for insulin production is removed. Regular follow-up appointments with the surgical team, oncologists, and nutritionists are essential to manage these potential long-term effects and ensure the best possible quality of life.