Radical Prostatectomy
Radical Prostatectomy is a surgical procedure primarily used to treat localized prostate cancer. This article aims to provide a comprehensive understanding of the procedure, its recovery process, and potential side effects, offering valuable information for patients and their families.
Key Takeaways
- Radical Prostatectomy involves the surgical removal of the entire prostate gland and surrounding tissues, typically for early-stage prostate cancer.
- The procedure can be performed using open surgery or minimally invasive techniques, such as laparoscopic or robotic-assisted methods.
- Recovery after Radical Prostatectomy includes a hospital stay, temporary catheter use, and a gradual return to normal activities, with full recovery spanning several weeks to months.
- Common potential side effects Radical Prostatectomy include urinary incontinence and erectile dysfunction, which often improve over time but may require ongoing management.
- Pre-operative counseling and post-operative rehabilitation are crucial for managing expectations and optimizing long-term outcomes.
What is Radical Prostatectomy and How is it Performed?
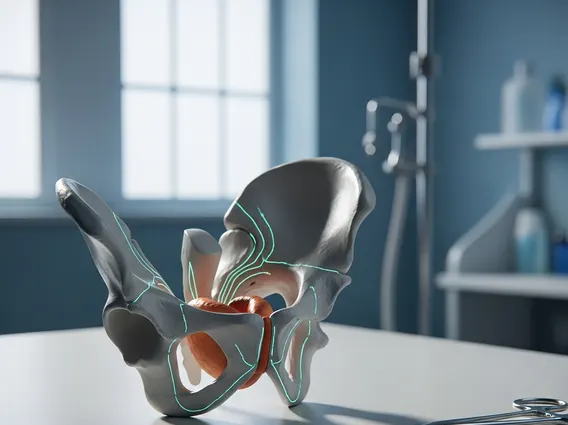
Radical Prostatectomy refers to a major surgical operation to remove the entire prostate gland, along with some surrounding tissue, including the seminal vesicles and, in some cases, nearby lymph nodes. This procedure is a common treatment option for men diagnosed with localized prostate cancer, meaning the cancer is confined to the prostate and has not spread to other parts of the body. The decision to undergo this surgery is made after careful consideration of the cancer’s aggressiveness, the patient’s overall health, and potential treatment outcomes.
The radical prostatectomy procedure can be performed using several surgical approaches, each with its own advantages and considerations. According to the American Cancer Society, prostate cancer is the second most common cancer in American men, with about 1 in 8 men being diagnosed during their lifetime, highlighting the prevalence of such treatments. The primary goal of the surgery is to remove all cancerous tissue while preserving urinary and sexual function as much as possible. The main types of surgical approaches include:
- Open Radical Prostatectomy: This traditional method involves a single incision in the lower abdomen to access and remove the prostate gland.
- Laparoscopic Radical Prostatectomy: A minimally invasive approach where several small incisions are made, and specialized instruments, along with a camera, are inserted to perform the surgery.
- Robotic-Assisted Laparoscopic Radical Prostatectomy: This is the most common minimally invasive technique, utilizing a robotic system controlled by the surgeon to enhance precision and dexterity through small incisions.
Each approach aims to achieve the same outcome but differs in terms of recovery time, blood loss, and potential impact on surrounding nerves. The choice of technique often depends on the surgeon’s experience, the patient’s anatomy, and the specific characteristics of the cancer.
Recovery and Potential Side Effects of Radical Prostatectomy
Recovery after Radical Prostatectomy is a gradual process that varies among individuals, typically requiring a hospital stay of a few days. Patients will have a urinary catheter in place for one to three weeks post-surgery to allow the urethra to heal. During this period, activities are restricted, and patients are advised to avoid heavy lifting and strenuous exercise. Most men can return to light activities within a few weeks, but full recovery, including the return of strength and energy, can take several months. Post-operative care often includes pelvic floor exercises (Kegel exercises) to help regain bladder control.
The most common and significant side effects Radical Prostatectomy are urinary incontinence and erectile dysfunction. These side effects occur because the prostate gland is located close to nerves that control erections and the sphincter muscle that controls urination. While surgical techniques aim to preserve these structures, some degree of impact is often unavoidable. Studies indicate that a significant percentage of men experience some degree of urinary incontinence and erectile dysfunction following radical prostatectomy, though rates and severity vary widely based on surgical technique, patient factors, and post-operative rehabilitation. For instance, a systematic review published in European Urology found that rates of erectile dysfunction range from 30% to 80% and urinary incontinence from 5% to 30% at one year post-surgery, depending on the definition and assessment methods.
Other potential side effects, though less common, can include:
- Changes in orgasm (e.g., dry orgasm due to removal of seminal vesicles).
- Shortening of the penis.
- Lymphedema (swelling in the legs or genital area if lymph nodes are removed).
- Bowel problems (rare).
Many of these side effects improve over time with rehabilitation and medical management. For urinary incontinence, options range from pelvic floor therapy to medications or, in some cases, further surgical interventions. For erectile dysfunction, treatments include oral medications, vacuum devices, injections, or penile implants. Open communication with the healthcare team is essential for managing these challenges and optimizing the quality of life after surgery.