Pelvic Wall
The Pelvic Wall is a critical anatomical structure forming the boundaries of the pelvic cavity, providing essential support and protection for the organs housed within. Understanding its composition and function is fundamental to comprehending various aspects of human health and common medical conditions.
Key Takeaways
- The Pelvic Wall is a complex structure of muscles, ligaments, and fascia that forms the floor and sides of the bony pelvis.
- It plays a vital role in supporting pelvic organs, maintaining continence, and facilitating childbirth.
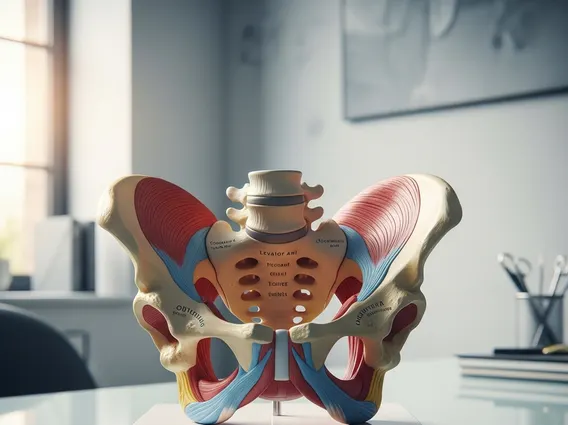
- Key muscles include the levator ani group, coccygeus, obturator internus, and piriformis.
- Dysfunction or injury to the pelvic wall can lead to various symptoms, including pain and organ prolapse.
- Causes of pelvic wall pain are diverse, ranging from musculoskeletal issues to neurological conditions and inflammatory processes.
What is the Pelvic Wall?
The Pelvic Wall refers to the muscular and ligamentous structures that form the inferior (floor) and lateral (side) boundaries of the true pelvis. This intricate anatomical arrangement is crucial for supporting the abdominal and pelvic viscera, maintaining continence, and providing stability to the trunk. It is composed of several layers of muscles, fascia, and connective tissues that stretch across the bony framework of the pelvis, creating a dynamic and supportive sling.
This robust structure acts as a foundation, preventing the downward displacement of organs such as the bladder, uterus (in females), prostate (in males), and rectum. Its integrity is paramount for normal physiological functions, and any compromise can lead to significant health issues, including pelvic organ prolapse or various forms of pelvic pain.
Pelvic Wall Anatomy and Function
The anatomy of the pelvic wall is complex, involving several muscles that originate from the pelvic bones and converge to form a resilient diaphragm. The primary muscles of the pelvic wall are broadly categorized into the pelvic diaphragm and the lateral wall muscles. The pelvic diaphragm, which forms the floor, consists mainly of the levator ani group (puborectalis, pubococcygeus, iliococcygeus) and the coccygeus muscle. These muscles create a funnel-shaped structure with an opening for the urethra, vagina (in females), and rectum.
Beyond support, the pelvic wall performs several critical functions:
- Organ Support: It provides a strong hammock-like support for the pelvic organs, counteracting intra-abdominal pressure.
- Continence: The muscles, particularly the puborectalis part of the levator ani, contribute significantly to urinary and fecal continence by maintaining tone around the urethra and anal canal.
- Childbirth: During labor, the pelvic wall muscles relax and stretch to allow the passage of the baby through the birth canal.
- Core Stability: It works in conjunction with the abdominal muscles and diaphragm to stabilize the trunk and facilitate efficient movement.
The lateral walls of the pelvis are formed by the obturator internus and piriformis muscles, which also contribute to hip movement and stability. These muscles are covered by strong fascial layers that further reinforce the pelvic structure.
Causes of Pelvic Wall Pain
Pelvic wall pain causes are diverse and can stem from musculoskeletal, neurological, inflammatory, or organ-related issues. Chronic pelvic pain, which often involves the pelvic wall, affects a significant portion of the population, with estimates suggesting up to 15-20% of women globally experience it at some point, according to data from organizations like the World Health Organization (WHO).
Common causes include:
- Musculoskeletal Dysfunction: Overuse, injury, or chronic tension in the pelvic floor muscles (e.g., levator ani spasm, myofascial pain syndrome) can lead to localized or referred pain.
- Nerve Entrapment: Nerves passing through or near the pelvic wall, such as the pudendal nerve or obturator nerve, can become compressed or irritated, causing neuropathic pain.
- Pelvic Organ Prolapse: Weakness in the pelvic wall can lead to the descent of pelvic organs (e.g., bladder, uterus, rectum), causing a sensation of pressure, discomfort, or pain.
- Inflammatory Conditions: Conditions like endometriosis, interstitial cystitis, or inflammatory bowel disease can cause inflammation that irritates nearby pelvic wall structures.
- Post-Surgical Pain: Adhesions or nerve damage following pelvic surgeries can contribute to persistent pain in the region.
Diagnosis often involves a thorough physical examination, imaging studies, and sometimes nerve blocks to identify the specific source of pain. Effective management typically requires a multidisciplinary approach tailored to the underlying cause.