Cystic Fibrosis
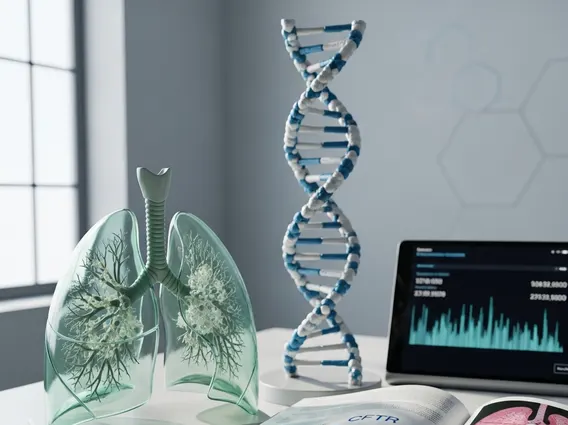
Cystic Fibrosis is a serious genetic disorder that impacts multiple organs, primarily the lungs and digestive system, by causing the production of thick, sticky mucus. Understanding this condition is crucial for managing its effects and improving patient outcomes.
Key Takeaways
- Cystic Fibrosis (CF) is an inherited genetic disorder affecting exocrine glands, leading to thick mucus production.
- It primarily impacts the respiratory and digestive systems, causing persistent cough, breathing difficulties, and malabsorption.
- The condition is caused by mutations in the CFTR gene, which regulates salt and water transport in cells.
- Treatment focuses on managing symptoms, preventing complications, and improving quality of life through a multidisciplinary approach.
- Advances in CFTR modulator therapies are targeting the underlying genetic defect.
What is Cystic Fibrosis (CF)?
Cystic Fibrosis (CF) is a progressive, inherited genetic disorder that causes severe damage to the lungs, digestive system, and other organs in the body. It affects the cells that produce mucus, sweat, and digestive juices. Normally, these secreted fluids are thin and slippery. However, in individuals with CF, a defective gene causes the secretions to become thick and sticky. Instead of acting as lubricants, they plug up tubes, ducts, and passageways, especially in the lungs and pancreas.
This buildup of thick mucus in the lungs can lead to persistent lung infections and breathing problems. In the digestive system, it can block the ducts of the pancreas, preventing digestive enzymes from reaching the small intestine, which impairs the body’s ability to break down food and absorb vital nutrients. According to the Cystic Fibrosis Foundation, more than 30,000 children and adults in the United States live with cystic fibrosis, and approximately 1,000 new cases are diagnosed each year.
Symptoms and Genetic Causes of Cystic Fibrosis
The signs and cystic fibrosis symptoms vary depending on the severity of the disease and the organs affected. Common respiratory symptoms include a persistent cough that produces thick mucus, wheezing, shortness of breath, and recurrent lung infections like bronchitis or pneumonia. Digestive symptoms often involve poor weight gain and growth despite a good appetite, severe constipation, and greasy, foul-smelling stools due to malabsorption.
The fundamental causes of cystic fibrosis lie in a mutation within the cystic fibrosis transmembrane conductance regulator (CFTR) gene. This gene provides instructions for making the CFTR protein, which acts as a channel across the membrane of cells that produce mucus, sweat, saliva, tears, and digestive enzymes. The CFTR protein is responsible for transporting chloride ions, which helps regulate the movement of water in tissues. When the CFTR gene is mutated, the protein either doesn’t work correctly or isn’t produced at all. This disruption leads to an imbalance of salt and water, resulting in the characteristic thick, sticky mucus and salty sweat.
Cystic fibrosis is an autosomal recessive genetic disorder, meaning a child must inherit two copies of the defective CFTR gene—one from each parent—to develop the condition. If a child inherits only one copy, they are a carrier and typically do not show symptoms but can pass the gene to their own children.
Cystic Fibrosis Treatment Options
While there is currently no cure for cystic fibrosis, significant advancements in cystic fibrosis treatment options have dramatically improved the quality of life and life expectancy for individuals with the condition. Treatment strategies are comprehensive and aim to manage symptoms, prevent complications, and address the underlying genetic defect. A multidisciplinary team, including pulmonologists, gastroenterologists, nutritionists, and physical therapists, typically provides care.
Key treatment approaches include:
- Airway Clearance Techniques (ACTs): These methods help loosen and clear the thick mucus from the lungs. Examples include chest physical therapy, vibrating vests, and breathing exercises.
- Medications: This category includes bronchodilators to open airways, mucolytics (mucus thinners) to make mucus easier to cough up, anti-inflammatory drugs to reduce lung inflammation, and antibiotics to treat and prevent lung infections.
- CFTR Modulators: These groundbreaking drugs target the defective CFTR protein itself, helping it to function more effectively. They are designed for specific CFTR gene mutations and can significantly improve lung function and reduce exacerbations.
- Nutritional Support: Pancreatic enzyme supplements are taken with meals to aid digestion and nutrient absorption. High-calorie, high-fat diets and vitamin supplements are often recommended to combat malnutrition.
- Lung Transplant: For individuals with severe lung damage and advanced disease, a lung transplant may be a viable option to improve breathing and overall health.
It is important to note that any information regarding supportive or complementary therapies should not replace conventional medical treatment and should always be discussed with a healthcare provider.
