Total Parenteral Nutrition
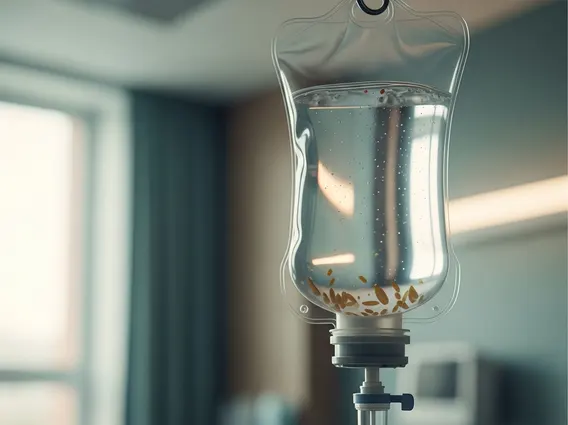
Total Parenteral Nutrition (TPN) is a critical medical intervention providing complete nutritional support intravenously. It is employed when a patient’s gastrointestinal tract is unable to digest or absorb nutrients adequately.
Key Takeaways
- Total Parenteral Nutrition (TPN) delivers all essential nutrients directly into the bloodstream, bypassing the digestive system.
- TPN is indicated for patients who cannot receive adequate nutrition orally or enterally due to various medical conditions.
- It provides a balanced mix of carbohydrates, proteins, fats, vitamins, minerals, and electrolytes.
- While life-sustaining, TPN carries potential risks, including infection, metabolic imbalances, and liver complications.
- Close medical monitoring is essential for patients receiving TPN to manage its benefits and mitigate side effects.
What is Total Parenteral Nutrition (TPN)?
Total Parenteral Nutrition (TPN) refers to a method of feeding that provides all the necessary nutrients directly into the bloodstream, bypassing the digestive system entirely. This complex nutritional solution is administered through a central venous catheter, typically placed in a large vein in the chest. A comprehensive understanding of total parenteral nutrition explained involves recognizing that it delivers a precise mixture of carbohydrates (as dextrose), proteins (as amino acids), fats (as lipid emulsions), electrolytes, vitamins, and trace minerals tailored to meet the individual patient’s metabolic needs.
TPN is a life-sustaining therapy for individuals whose gastrointestinal tract is non-functional or requires prolonged rest. It ensures that the body receives sufficient energy and building blocks for cellular function, tissue repair, and overall metabolic balance, preventing malnutrition and supporting recovery from illness or surgery.
Indications for Total Parenteral Nutrition (TPN)
The uses of total parenteral nutrition are diverse, primarily indicated for patients who cannot tolerate or absorb nutrients via the oral or enteral (tube feeding) routes for an extended period. This can be due to a variety of severe gastrointestinal conditions or other medical circumstances that preclude normal digestion and absorption. The decision to initiate TPN is made after careful evaluation by a healthcare team, considering the patient’s nutritional status, prognosis, and the expected duration of therapy.
Common indications for TPN include:
- Severe malabsorption syndromes (e.g., short bowel syndrome, Crohn’s disease with extensive bowel resection).
- Intestinal obstruction or ileus where the bowel is not functioning.
- High-output enterocutaneous fistulas, which prevent nutrient absorption.
- Severe pancreatitis requiring complete bowel rest.
- Prolonged inability to eat due to severe nausea, vomiting, or dysphagia (difficulty swallowing).
- Critical illness or severe burns where metabolic demands are extremely high and enteral feeding is not feasible.
Potential Side Effects of Total Parenteral Nutrition (TPN)
While TPN is a vital therapy, it is associated with several potential complications that require vigilant monitoring and management. Understanding total parenteral nutrition side effects is crucial for patient safety and optimizing outcomes. These complications can range from mild metabolic disturbances to severe, life-threatening conditions.
The primary categories of TPN-related side effects include:
- Infectious Complications: Catheter-related bloodstream infections (CRBSIs) are a significant risk due to the presence of a central venous catheter. Strict aseptic techniques during insertion and maintenance are essential to minimize this risk.
- Metabolic Complications: These can include hyperglycemia (high blood sugar), hypoglycemia (low blood sugar, especially upon abrupt cessation of TPN), electrolyte imbalances (e.g., potassium, magnesium, phosphate), and liver dysfunction (TPN-associated liver disease), which can manifest as elevated liver enzymes or cholestasis.
- Mechanical Complications: These are related to the central venous catheter insertion and can include pneumothorax (collapsed lung), hemothorax (blood in the chest cavity), arterial puncture, or catheter malposition. Catheter occlusion or dislodgement can also occur during therapy.
- Gastrointestinal Complications: Prolonged bowel rest can lead to gut atrophy, potentially increasing the risk of bacterial translocation and sepsis once oral feeding is resumed.
Regular blood tests, clinical assessments, and careful adjustment of the TPN formula are necessary to detect and manage these potential side effects effectively, ensuring the patient receives the maximum benefit with minimal risk.
