Subarachnoid Block
Subarachnoid Block, often referred to as spinal anesthesia, is a widely utilized regional anesthetic technique that provides temporary loss of sensation and motor function in a specific area of the body. This method is crucial in various surgical and obstetric procedures, offering an alternative to general anesthesia.
Key Takeaways
- Subarachnoid Block is a regional anesthetic technique involving injection into the cerebrospinal fluid (CSF) to block spinal nerves.
- It provides rapid onset of dense sensory and motor block, making it suitable for lower body surgeries.
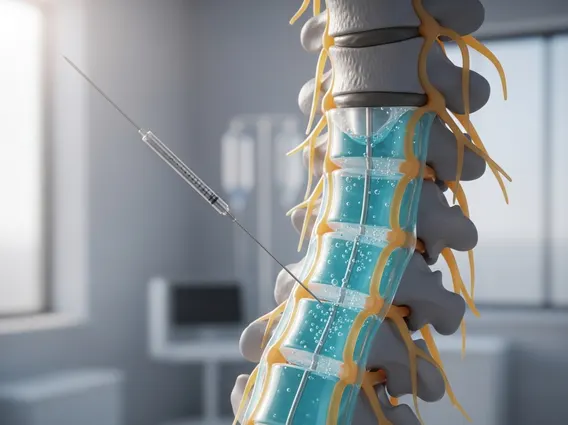
- The procedure involves careful needle placement in the subarachnoid space, typically below the L2 vertebral level.
- Common risks include hypotension, post-dural puncture headache, and transient neurological symptoms.
- Unlike epidural anesthesia, Subarachnoid Block uses a single, smaller dose directly into the CSF, resulting in a quicker, more profound block.
What is Subarachnoid Block?
Subarachnoid Block is a form of regional anesthesia achieved by injecting a local anesthetic solution into the subarachnoid space, which contains cerebrospinal fluid (CSF) and surrounds the spinal cord. This direct injection allows the anesthetic to quickly interact with the spinal nerves, blocking nerve impulses and resulting in a rapid onset of sensory and motor blockade. It is a highly effective method for numbing specific areas of the body, particularly the lower abdomen, pelvis, and lower extremities, while the patient remains conscious.
The primary mechanism involves the local anesthetic binding to voltage-gated sodium channels in the nerve membranes, preventing the generation and conduction of action potentials. This interruption of nerve signals leads to a temporary loss of sensation (analgesia) and muscle movement (motor block) in the regions innervated by the affected spinal nerves. The extent and duration of the block depend on the type and dose of anesthetic used, as well as patient-specific factors.
Subarachnoid Block Procedure, Uses, and Risks
The **Subarachnoid block procedure explained** involves several meticulous steps to ensure patient safety and efficacy. Typically, the patient is positioned either sitting or lying on their side with their back flexed to open the intervertebral spaces. After thorough skin preparation with an antiseptic solution and local anesthetic infiltration at the injection site, a fine needle is carefully inserted between the vertebrae, usually at the L3-L4 or L4-L5 interspace, below the termination of the spinal cord. Confirmation of correct placement is indicated by the free flow of cerebrospinal fluid (CSF) from the needle hub. Once confirmed, the local anesthetic is slowly injected.
The **Subarachnoid block uses and risks** are important considerations. This technique is widely used for various surgical procedures due to its effectiveness and ability to avoid the systemic effects of general anesthesia. Common surgical applications include:
- Cesarean sections and other obstetric procedures
- Lower limb surgeries (e.g., hip or knee replacement, ankle surgery)
- Urological procedures (e.g., transurethral resection of the prostate)
- Hernia repairs and other lower abdominal surgeries
- Perineal and anal surgeries
Despite its benefits, potential risks are associated with Subarachnoid Block. These can include a drop in blood pressure (hypotension) due to sympathetic blockade, a post-dural puncture headache (PDPH) caused by CSF leakage, and in rare cases, nerve injury, infection, or total spinal anesthesia. Careful patient selection, proper technique, and vigilant monitoring help mitigate these risks. According to a study published in the journal Anesthesiology, the incidence of severe neurological complications following spinal anesthesia is exceedingly low, estimated at less than 1 in 10,000 procedures.
Subarachnoid Block vs. Epidural Anesthesia
While both Subarachnoid Block and epidural anesthesia are regional anesthetic techniques targeting the spinal nerves, they differ significantly in their approach, onset, and characteristics. Understanding these distinctions is crucial for clinicians in selecting the most appropriate method for a given patient and procedure. The primary difference lies in the location of anesthetic delivery.
The comparison of **Subarachnoid block vs epidural** highlights their unique profiles:
| Feature | Subarachnoid Block (Spinal Anesthesia) | Epidural Anesthesia |
|---|---|---|
| Injection Site | Subarachnoid space (into CSF) | Epidural space (outside dura mater) |
| Needle Size | Typically finer gauge (e.g., 25-27G) | Larger gauge (e.g., 17-18G) |
| Onset of Block | Rapid (within 2-5 minutes) | Slower (10-20 minutes) |
| Density of Block | Dense sensory and motor block | Variable, often less dense; can be titrated |
| Dose Volume | Small volume (e.g., 2-4 mL) | Larger volume (e.g., 10-20 mL), often continuous infusion |
| Duration | Limited (2-4 hours, depending on drug) | Can be prolonged with catheter and infusion |
| Catheter Placement | Rarely used (single shot common) | Common for continuous analgesia/anesthesia |
| Risk of PDPH | Higher due to dural puncture | Lower, but still possible with accidental dural puncture |
Subarachnoid Block provides a more immediate and profound block, making it ideal for procedures requiring a rapid onset of complete anesthesia. Epidural anesthesia, conversely, allows for more gradual titration and prolonged pain control, often favored for labor analgesia or extended surgical procedures where a catheter can be left in place for continuous drug delivery.
