Cordotomy
Cordotomy is a neurosurgical procedure performed to alleviate severe, intractable pain, typically when other pain management strategies have proven ineffective. It involves precisely severing specific nerve pathways in the spinal cord responsible for transmitting pain signals to the brain.
Key Takeaways
- Cordotomy is a neurosurgical procedure targeting specific pain pathways in the spinal cord.
- It is primarily indicated for patients suffering from severe, intractable chronic pain, often associated with cancer.
- The procedure aims to provide significant pain relief by interrupting pain signal transmission.
- While effective, it carries potential risks and benefits that must be carefully weighed by patients and their medical teams.
What is Cordotomy?
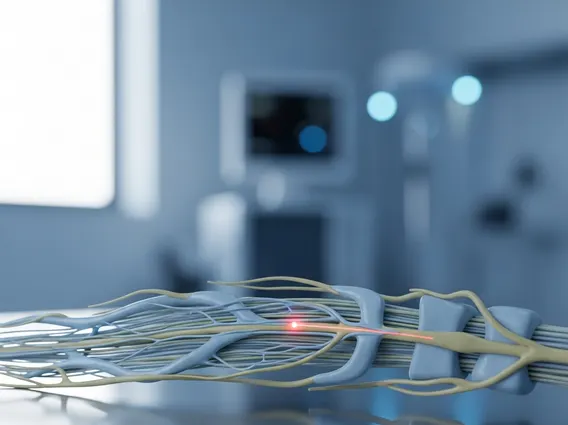
Cordotomy refers to a surgical intervention that involves making a lesion in the spinothalamic tract of the spinal cord. This tract is a crucial ascending pathway responsible for transmitting pain and temperature sensations from the body to the brain. By selectively interrupting these fibers, the procedure aims to block the transmission of pain signals from a specific part of the body, thereby providing significant pain relief to the patient. It is typically considered a last resort for individuals experiencing severe, debilitating pain that has not responded to conventional treatments.
Cordotomy Procedure and Indications for Chronic Pain
The **cordotomy procedure explained** typically involves a neurosurgeon creating a small lesion in the anterolateral quadrant of the spinal cord. This can be performed using different techniques, most commonly percutaneously (through the skin) under local anesthesia with fluoroscopic or CT guidance, or less frequently, via an open surgical approach. During the percutaneous procedure, a specialized electrode is inserted into the spinal cord to precisely locate and then ablate the pain-transmitting fibers. Patient cooperation is often crucial during the procedure to confirm the exact area of pain relief and avoid motor or other sensory deficits.
The primary indication for **cordotomy for chronic pain** is severe, unilateral, intractable pain, most often associated with advanced cancer. This type of pain is typically localized to one side of the body and is not adequately controlled by pharmacological or other less invasive methods. Candidates for cordotomy often have a limited life expectancy, making the immediate and effective pain relief offered by the procedure highly valuable for improving their quality of life in their remaining time. It is less commonly used for non-cancer pain due to the availability of other long-term pain management strategies and potential side effects.
Risks and Benefits of Cordotomy
Understanding the **cordotomy risks and benefits** is crucial for informed decision-making. The primary benefit of cordotomy is the potential for significant and often immediate relief from severe, intractable pain, which can dramatically improve a patient’s quality of life, mobility, and ability to participate in daily activities. For many patients, it offers a level of pain control unattainable through medication alone, reducing reliance on high-dose opioids and their associated side effects.
However, like any neurosurgical procedure, cordotomy carries potential risks. These can vary depending on the technique used and the patient’s overall health. Potential complications include:
- Temporary or permanent weakness (motor deficit) on the same side as the pain relief.
- Sensory changes, such as numbness or altered sensation, in areas beyond the intended pain relief zone.
- Bladder or bowel dysfunction, though rare, especially with bilateral procedures.
- Mirror pain, where pain develops on the opposite side of the body.
- Dysesthesia (unpleasant abnormal sensation) or neuropathic pain in the area of pain relief.
- Respiratory difficulties, particularly with lesions high in the cervical spine, which can affect breathing muscles.
Due to these potential complications, cordotomy is carefully considered and performed only after a thorough evaluation by a multidisciplinary pain management team, ensuring that the potential benefits outweigh the risks for the individual patient.